Articles
- Page Path
- HOME > Kosin Med J > Volume 38(2); 2023 > Article
-
Original article
Dietary education may reduce blood cadmium and mercury levels in chronic kidney disease patients with higher blood cadmium and mercury levels -
Su Mi Lee1
 , Young-Seoub Hong2,3
, Young-Seoub Hong2,3 , Byoung-Gwon Kim2,3
, Byoung-Gwon Kim2,3 , Jung-Yeon Kwon2
, Jung-Yeon Kwon2 , Yongsoon Park4
, Yongsoon Park4 , Seong Eun Kim1
, Seong Eun Kim1 , Won Suk An1
, Won Suk An1
-
Kosin Medical Journal 2023;38(2):107-116.
DOI: https://doi.org/10.7180/kmj.23.101
Published online: May 24, 2023
1Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea
2Environmental Health Center, Dong-A University, Busan, Korea
3Department of Preventive Medicine, Dong-A University College of Medicine, Busan, Korea
4Department of Food and Nutrition, Hanyang University, Seoul, Korea
- Corresponding Author: Won Suk An, MD, PhD Department of Internal Medicine, Dong-A University, 32 Daesingongwon-ro, Seo-gu, Busan 49201, Korea Tel: +82-51-240-2811 Fax: +82-51-242-5852 E-mail: anws@dau.ac.kr
Copyright © 2023 Kosin University College of Medicine.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,359 Views
- 44 Download
- 1 Crossref
Abstract
-
Background
- Exposure to cadmium and mercury is associated with renal dysfunction. This study aimed to investigate the possible ability of dietary education to decrease blood cadmium and mercury levels in patients with chronic kidney disease (CKD).
-
Methods
- Twenty-seven patients with CKD were enrolled in this prospective, single-arm pilot study. Patients with blood cadmium levels ≥1.4 μg/L were instructed to reduce their intake of shellfish, while those with blood mercury levels ≥5.0 μg/L were asked to reduce their intake of externally blue-colored fish.
-
Results
- Seven dialysis patients and 15 pre-dialysis patients completed the study. Compared with baseline, the blood cadmium (2.0±0.7 μg/L vs. 1.8±0.7 μg/L, p=0.031) and mercury levels (4.4±2.6 μg/L vs. 3.5±1.9 μg/L, p=0.005) after 1 year significantly decreased, although the dietary intake was not significantly different in patients with blood cadmium levels ≥1.4 μg/L and blood mercury levels ≥5.0 μg/L. In pre-dialysis patients, kidney function worsened after 1 year compared with that at baseline despite the reduction in blood cadmium and mercury levels.
-
Conclusions
- Reduction of food intake containing cadmium and mercury may lower the blood cadmium and mercury levels in CKD patients with higher cadmium and mercury levels. Higher blood cadmium levels may cause renal disease progression in pre-dialysis patients, and further studies are necessary to determine the underlying mechanisms.
- Chronic kidney disease (CKD) is a growing public health concern, and diabetes mellitus (DM), hypertension, and glomerulonephritis are known to be the main causes of CKD. Heavy metals can be considered an unfamiliar cause of CKD, especially when there are no definite etiologies of CKD [1]. Cadmium (Cd) is a heavy metal that causes renal tubular dysfunction and cardiovascular disease [2-4]. In hemodialysis (HD) patients, blood Cd level is one of the risk factors affecting mortality [5]. A recent cross-sectional study reported that Cd exposure was also risk factor for development and progression of CKD, particularly in vulnerable populations with hypertension or DM [6]. Therefore, the role of Cd exposure and Cd levels in the occurrence of CKD should not be neglected.
- The primary source of human mercury (Hg) exposure is ingestion of food contaminated with Hg because Hg is readily absorbed by the gastrointestinal tract. Inorganic and organic forms of Hg readily accumulate in the kidney and may induce acute kidney injury by inorganic forms of Hg intoxication [7,8]. Epidemiologic studies investigating the relationship between CKD and Hg exposure are limited [9,10]. The exposed individuals with blood Hg levels ≥5.0 μg/L showed higher urine protein and higher serum creatinine levels than those with blood Hg levels <5.0 μg/L at Bibiani Ghana [11]. Efforts to lower or not increase until the Hg level (5.0 μg/L) suggested in the World Health Organization (WHO) guideline are important.
- Toxic heavy metals are widely distributed and tend to accumulate in the environment. Dietary exposure is one of the primary causes of toxic heavy metal accumulation in the human body. The major source of dietary Cd intake is shellfish consumption, and Cd burdens are higher in the seaside areas of Korea [12]. Another study showed that blood Hg concentrations increased with increasing annual fish consumption such as mackerel and tuna [13]. This study was designed to identify whether blood Cd and Hg levels can be lowered through dietary education in CKD patients. We also aimed to analyze the changes in kidney function and proteinuria in patients with pre-dialysis CKD.
Introduction
- Ethical statements: The protocol was approved by the Institutional Review Board of Dong-A University Hospital (IRB No. DAUHIRB-17-199) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent to participate was obtained from all participants.
- 1. Study design and population
- We conducted a prospective, single-arm, pilot study of patients with CKD from December 2017 to September 2020. Twenty-seven CKD patients including seven dialysis patients with baseline blood Cd levels ≥1.4 μg/L or blood Hg levels ≥5.0 μg/L were enrolled. The cutoff value for blood Hg level was determined based on the WHO guidelines, while that for blood Cd level was determined based on the mean blood Cd level in 128 Korean CKD patients [6].
- Patients with baseline blood Cd levels <1.4 μg/L and blood Hg levels <5.0 μg/L, those who did not receive dietary education or did not participate in a nutrition survey, and those who had no caregivers to prepare their meals were excluded.
- The primary outcome was the change in blood Cd and Hg levels. The secondary outcomes included changes in renal function and proteinuria in the pre-dialysis patients. All enrolled patients were asked about their average food consumption frequency and portion size of food consumed at the initiation of the study and after 1 year.
- 2. Survey of nutrition
- The survey was conducted using a semiquantitative food frequency questionnaire targeting 121 foods. The patients’ nutritional intake was estimated using the Computer-Aided Nutritional Analysis Program (Can-Pro 3.0, The Korean Nutrition Society), which includes data on 1,823 foods.
- All participants were requested to prepare a meal diary, which can be used for dietary education, a month before visiting the outpatient clinic. For example, patients with high blood Cd levels recorded the type and quantity of shellfish consumed for a month, while those with high blood Hg levels recorded the type and quantity of fish consumed for a month.
- 3. Dietary education
- Dietary education was conducted every 3 to 4 months, and at least three outpatient visits were required per year. The dietary education was implemented as follows.
- Fish intake was evaluated, and the patients were asked to reduce the intake by 50%. If the patients consumed fish twice a week, they were instructed to reduce the intake to once a week or to consume half of their usual intake. Even if patients consumed fish less than once a week, they were still asked to reduce their intake by 50%. Moreover, if the patients ate less quantity of fish, they were still asked to reduce their intake of fish and shellfish by 50% after evaluating the usual amount of fish and shellfish that they consume.
- Shellfish intake was assessed and the patients were asked to reduce the intake by 50%. If the patients consumed shellfish twice a week, they were instructed to reduce the intake of shellfish once a week or to consume half of their usual intake. Even if patients consumed shellfish less than once a week, they were still trained to reduce their intake by 50%. If the patients ate less quantity of fish or did not eat red meat more than once a week, the current intake of red meat was increased by 50% or the intake was doubled.
- 4. Analysis of blood Cd and Hg concentration
- Blood levels of Cd and Hg were measured at study initiation and 1 year later. In order to prevent clotting in blood samples, venous blood was obtained using 3-mL vacutainers (Beckton and Dickton) treated with ethylenediaminetetraacetic acid. A direct Hg analyzer (MA3000, NIC) was used to analyze the total blood Hg levels. To create a calibration curve, four reference samples including total blood (Hg 0.5–10 ppb) were prepared by diluting a standard solution (Waco Co.). When the linearity (r) of the calibration curve was less than 0.998, re-analysis was performed. The limit of detection was estimated to be 0.0021 ng. The analytical method of gold amalgamation was applied to determine the total Hg level in the blood according to the U.S. Environmental Protection Agency Method 7473 [14]. Commonly used standard agents were used to ensure the internal quality control and management of heavy metals: Whole Blood Metal Control Levels 1 and 2 (Seronorm, SERO AS) for measuring Hg levels in the blood. As a proof of external quality control and management, certifications for the analysis of total blood Hg levels were secured from the German External Quality Assessment Scheme (G-EQUAS) of Friedrich-Alexander University. Graphite furnace atomic absorption spectrometry with Zeeman background correction (900Z, Perkin-Elmer) was applied to determine the total Cd levels in the blood. To create a calibration curve, four reference samples including Cd in blood (0.5–4 ppb) were prepared by diluting a standard solution (SPEX CertiPrep). When the linearity (r) of the calibration curve was less than 0.998, re-analysis was performed. Commonly used standard agents were used to ensure the internal quality control and management of heavy metals: Whole Blood Metal Control Level 1 (Seronorm, SERO AS) and ClinChek Whole Blood Control Levels 1 and 2 (RECIPE Chemical) for blood Cd. As a proof of external quality control and management of heavy metals, certifications for the analysis of total blood Cd levels were secured from the G-EQUAS of Friedrich-Alexander University.
- 5. Laboratory measurements
- Serum levels of blood urea nitrogen, creatinine, albumin, hemoglobin, calcium, and phosphorus were checked at the beginning and end of the study in pre-dialysis and dialysis patients. Proteinuria was measured from random spot urine.
- 6. Statistical analysis
- Data are presented as mean±standard deviation, median (interquartile range), or frequency as appropriate. The nonparametric Wilcoxon signed-rank test was conducted to compare the baseline data with the data at 1 year. Statistical significance was set when the p-value was less than 0.05. The SPSS version 18.0 software (SPSS inc.) was used for statistical analysis.
Methods
1) In patients with blood Hg levels ≥5.0 μg/L
2) In patients with blood Cd levels ≥1.4 μg/L
- 1. Baseline characteristics and biochemical data
- Among the 27 CKD patients, four dropped out from the study and one withdrew consent. Twenty-two patients completed the trial within 1 year after receiving dietary education. The average age of patients was 64.3±9.9 years, 36.4% were male, 31.8% had DM, and 81.8% had hypertension. Six patients had a blood Cd level ≥1.4 μg/L and a blood Hg level ≥5.0 μg/L. Of the 15 pre-dialysis patients (63.6%), 14 had CKD stages 2–4, while one had CKD stage 5 without undergoing dialysis. Of the seven dialysis patients (36.4%), six underwent HD, while one underwent peritoneal dialysis.
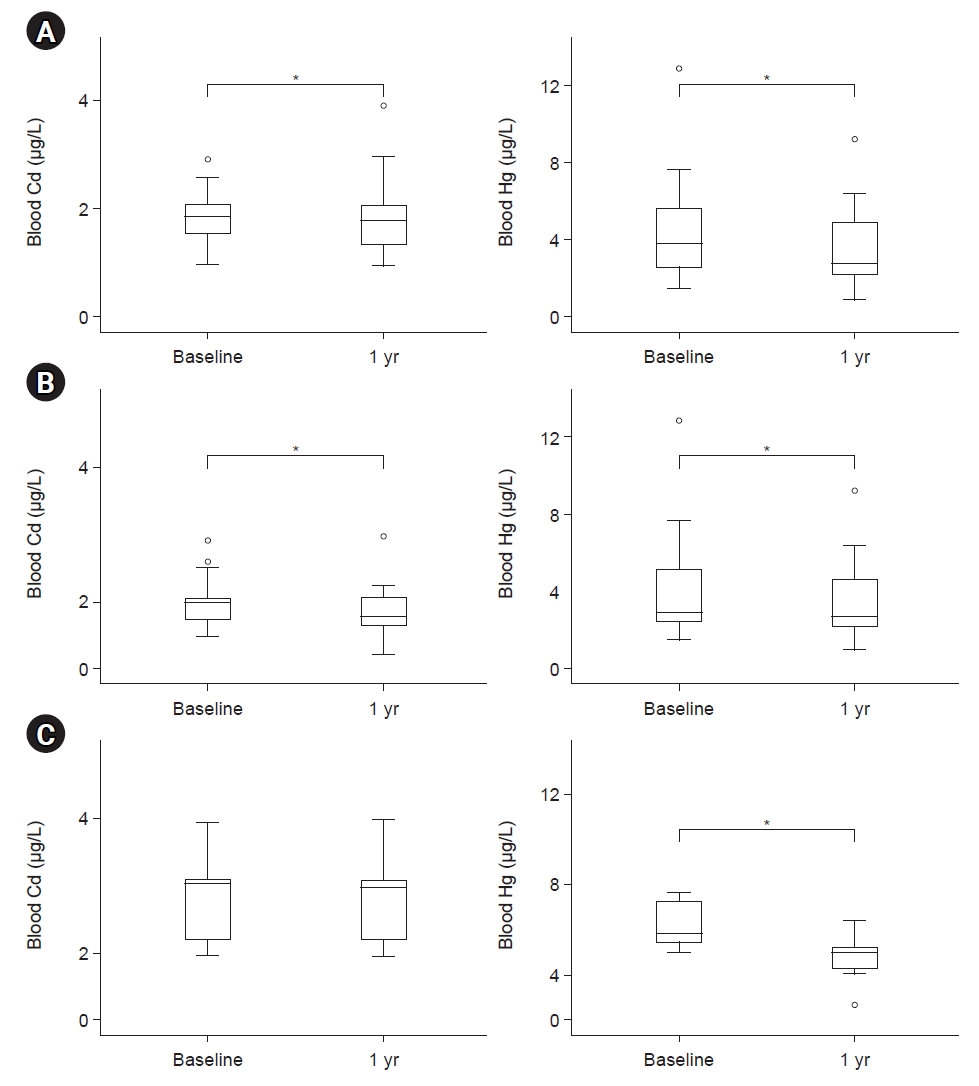
- The serum creatinine levels after 1 year were significantly increased, while the estimated glomerular filtration rate (eGFR) were significantly decreased compared with the baseline levels (Table 1). There were no patients with acute kidney injury. The blood Cd and Hg levels after 1 year were significantly decreased compared with the baseline levels in patients who completed this study (Fig. 1A).
- 2. Changes in diet
- For patients who completed this study, total calories and intake of each nutrient were analyzed at baseline and after 1 year of dietary education (Supplementary Table 1). No significant difference was observed in the nutrition status between the time points “before” and “1 year after dietary education.” However, dietary restrictions, such as consumption of fish and shellfish, have been imposed, presumably due to the reduced intake of animal protein and overall nutrients after a year.
- 3. Changes in biochemical data Laboratory measurements
- In patients with blood Cd levels ≥1.4 μg/L (n=19), the blood Hg and Cd levels after 1 year of dietary education were significantly decreased compared with baseline levels (Table 2, Fig. 1B). Dietary intakes were not different at baseline and after 1 year of dietary education, but the eGFR after 1 year were significantly decreased compared with the baseline levels in patients with blood Cd levels ≥1.4 μg/L.
- In pre-dialysis patients with blood Cd levels ≥1.4 μg/L (n=12), the blood Cd levels after 1 year were not significantly decreased, but the Hg levels after 1 year of dietary education were significantly decreased compared with the baseline levels; however, no significant difference was observed in terms of dietary intake (Supplementary Table 2). On the contrary, the serum creatinine and eGFR levels after 1 year of dietary education were significantly worse than the baseline levels. In dialysis patients, no significant difference was observed in the dietary intake as well as blood Cd and Hg levels after 1 year of dietary education compared with the baseline levels (Supplementary Table 3). In patients with blood Hg levels ≥5.0 μg/L (n=9), the blood Hg levels after 1 year were significantly decreased, but the Cd blood levels were not different compared with the baseline levels (Table 3, Fig. 1C). Although dietary intakes were not different at baseline and after 1 year of dietary education, renal function was not worse compared with that at baseline in patients with blood Hg levels ≥5.0 μg/L.
Results
- We found that dietary education to reduce fish and shellfish intake helped decrease the blood Cd and Hg levels in this pilot study. Generally, heavy metals accumulate in the body and are not removed from the body tissues. However, this study suggests the possibility of reducing Cd and Hg from the body tissue or at least not increasing human body accumulation by avoiding Cd- and Hg-containing foods. The Korea National Environmental Health Survey and Korea National Health and Nutrition Examination Survey (KNHANES) reported a heavy metal age-standardized geometric mean (GM) for blood Hg of 3.64 µg/L in 2008, which decreased to 2.92 µg/L in 2017 [15]. Based on the KNHANES data, the blood Cd levels of the general population also decreased from 0.93 µg/L in 2008 to 0.77 µg/L in 2017 [16]. These data also support that monitoring and correct handling of heavy metals may affect the blood Cd and Hg levels in the general population despite the wide distribution and accumulation of Cd and Hg in the environment. This pilot study demonstrated that reduction in the consumption of fish or shellfish may reduce the blood Cd and Hg levels even in CKD patients with reduced heavy metal excretion.
- Previous studies have shown that the GM of blood Hg levels was higher according to seafood intake, indicating an increase in Hg exposure [17,18]. Schober et al. [19] showed that the lowest Hg levels were found in the study group that did not consume seafood, and higher Hg levels were found in the study group that consumed seafood in the last 30 days. In Korea and Central Italy, the levels of Cd in the internal organs and tissues of shellfish, such as gastropod species, bay scallop, and comb pen shell were extremely high compared with those of Hg and Pb [20,21]. Hence, when eating shellfish, the internal organs must be removed to reduce Cd exposure. Both blood Cd and Hg levels were significantly reduced after 1 year in patients with blood Cd levels ≥1.4 μg/L. However, only blood Hg levels were significantly reduced, while the blood Cd levels remained unchanged after 1 year in patients with blood Hg levels ≥5.0 μg/L. Patients with blood Cd levels ≥1.4 μg/L were advised to reduce shellfish intake, while those with blood Hg levels ≥5.0 μg/L were advised to reduce intake of fish, such as mackerel. Although it is difficult to conclude that reducing shellfish intakes is more efficient in lowering Cd and Hg levels than reducing fish intakes, further studies are needed to identify various factors, including foods that can affect heavy metal levels.
- In this study, the blood Cd levels of enrolled CKD patients were higher than those of the general population based on the KNHANES data. Renal elimination of Cd is extremely slow, especially in CKD patients with low GFR. It is not surprising that the blood Cd levels of CKD patients in the pre-dialysis group with Cd levels ≥1.4 μg/L were higher than those of non-CKD and CKD patients in the 2011 KNHANES V-2 [6]. Cd can accumulate in the liver and kidney and may affect the functions of the kidney. Metallothioneins (MTs) are synthesized in the liver to form the Cd–MT complex. The Cd–MT complex filtered from the glomerulus and reabsorbed in segment 1 and segment 2 of the proximal tubules [22]. Cd has a long half-life, and nearly 50% of Cd accumulates in the kidney; the accumulated Cd reduces the GFR and induces tubular dysfunction [23,24]. Nephrotoxic Hg dose induces acute kidney injury with extensive tubular necrosis and tubular dysfunction in a CKD rat model with less residual renal function [25,26]. Therefore, patients with CKD are susceptible to the nephrotoxic effects of Hg. In this pilot study, the blood Hg levels of enrolled CKD patients were similar to those of non-CKD and CKD patients in the 2011 KNHANES V-2 [6]. The blood Hg levels may not be nephrotoxic even in CKD patients with blood Hg levels ≥5.0 μg/L. However, chronic exposure to higher Cd and Hg levels may lead to insults in CKD patients; hence, dietary education trials aimed at reducing the exposure to Cd and Hg may be helpful in improving the kidney health of CKD patients.
- It is peculiar that renal function based on eGFR (−2.7 mL/min/1.73 m2 per year) was significantly reduced after 1 year compared with that at baseline in pre-dialysis CKD patients with blood Cd levels ≥1.4 μg/L despite the reduction in blood Cd and Hg levels. Kidney Disease: Improving Global Outcomes guideline defines CKD as rapid progression when eGFR continuously decreases by more than 5 mL/min/1.73 m2 per year [27]. The rate of renal function reduction varies according to the severity of proteinuria and the presence of DM. In general, a GFR decline of approximately 0.3–1 mL/min/1.73 m2 per year is common among participants without proteinuria or comorbidity, and the deterioration in renal function is about two to three times faster among participants with proteinuria or comorbidities [28,29]. Factors such as age, diabetes, proteinuria, and hypertension of patients included in this study are considered to be factors of deterioration of renal function. Also, these patients had higher Cd and Hg levels, to these parts may have affected the deterioration of renal function. Blood Cd and Hg levels can indicate a relatively recent exposure and chronic exposure history [30]. Therefore, the recent reduction in blood Cd and Hg levels may not necessarily delay the progression of renal disorder. In other words, chronic exposure to Cd, which increases the blood Cd levels to ≥1.4 μg/L, may exacerbate the GFR decline in CKD patients with blood Cd levels ≥1.4 μg/L after 1 year. Reducing Cd level can be assumed that it can delay the deterioration of renal function, not preventing deterioration of renal function. This short-term study may give hint to removing additional risk factor of decreasing renal function. Besides Ca and Hg exposure, various environmental contaminants such as lead and arsenic cause deterioration of organ damage including kidney and liver. Hence, long-term clinical studies are necessary to determine nephrotoxic levels of heavy metals in the blood and reducing effect of heavy metals for renal protection.
- Our study has some strengths. First, this prospective study evaluated the changes in blood Cd and Hg levels after dietary education. Several previous studies were usually cross-sectional designs and investigated the levels of Cd and Hg in blood in association with the amount of fish and shellfish consumed. Second, this study demonstrated that CKD patients were susceptible to Cd and Hg exposure.
- There are some limitations to this study. First, this study included a relatively small number of patients and had a follow-up period of only 1 year. Second, the enrolled CKD patients were mixed according to CKD stage and dialysis status. Third, we did not assess the Cd levels in the urine or inorganic or organic Hg levels; we only evaluated the Cd and Hg levels in the blood after provision of dietary education. Fourth, a semiquantitative food frequency questionnaire was used to evaluate the patients’ diet at baseline and 1 year after provision of dietary education. It was not monitored using objective indicators to identify whether dietary education was being conducted properly at every visit.
- Dietary education to reduce food intake containing Cd and Hg may help lower the blood Cd and Hg levels in CKD patients with higher blood Cd and Hg levels. Further studies are necessary to determine whether active dietary education and interventions are helpful not only in patients with CKD but also in the general population with higher blood Cd and Hg levels. Still, higher blood Cd levels may affect renal progression in pre-dialysis CKD patients, and further large-scale studies are necessary to confirm this result.
Discussion
Supplementary material
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
This work was supported by grants from the Environmental Health Center, funded by the Ministry of Environment, Republic of Korea.
-
Author contributions
Conceptualization: WSA. Data curation: SML, YSH, BGK, JYK, YP, SEK, WSA. Methodology: SML, YSH, BGK, JYK, YP, SEK, WSA. Formal analysis: SML, WSA. Supervision: SML, YSH, BGK, JYK, YP, SEK, WSA. Writing – original draft: SML, WSA. Writing – review & editing: SML, WSA. Approval of final manuscript: all authors.
Article information
Values are presented as mean±standard deviation, number (%), or median (interquartile range).
BUN, blood urea nitrogen; eGFR, estimated glomerular filtration rate; UPCR, urinary protein to creatinine ratio.
The nonparametric Wilcoxon signed-rank was used to compare baseline data with 1-year data: p<0.05 (mean values are significantly different from the baseline levels).
Values are presented as mean±standard deviation or median (interquartile range).
BUN, blood urea nitrogen; eGFR, estimated glomerular filtration rate; UPCR, urinary protein to creatinine ratio.
The nonparametric Wilcoxon signed-rank was used to compare baseline data with 1-year data: p<0.05 (mean values are significantly different from the baseline levels).
Values are presented as mean±standard deviation or median (interquartile range).
BUN, blood urea nitrogen; eGFR, estimated glomerular filtration rate; UPCR, urinary protein to creatinine ratio.
The nonparametric Wilcoxon signed-rank was used to compare baseline data with 1-year data: p<0.05 (mean values are significantly different from the baseline levels).
- 1. Lunyera J, Mohottige D, Von Isenburg M, Jeuland M, Patel UD, Stanifer JW. CKD of uncertain etiology: a systematic review. Clin J Am Soc Nephrol 2016;11:379–85.ArticlePubMedPMC
- 2. Jarup L, Berglund M, Elinder CG, Nordberg G, Vahter M. Health effects of cadmium exposure: a review of the literature and a risk estimate. Scand J Work Environ Health 1998;24 Suppl 1:1–51.PubMed
- 3. Jarup L, Akesson A. Current status of cadmium as an environmental health problem. Toxicol Appl Pharmacol 2009;238:201–8.ArticlePubMed
- 4. Faroon O, Ashizawa A, Wright S, Tucker P, Jenkins K, Ingerman L, et al. Toxicological profile for cadmium. Agency for Toxic Substances and Disease Registry (US); 2012.
- 5. Hsu CW, Yen TH, Chen KH, Lin-Tan DT, Lin JL, Weng CH, et al. Effect of blood cadmium level on mortality in patients undergoing maintenance hemodialysis. Medicine (Baltimore) 2015;94:e1755.ArticlePubMedPMC
- 6. Kim NH, Hyun YY, Lee KB, Chang Y, Ryu S, Oh KH, et al. Environmental heavy metal exposure and chronic kidney disease in the general population. J Korean Med Sci 2015;30:272–7.ArticlePubMedPMCPDF
- 7. Emanuelli T, Rocha JB, Pereira ME, Porciuncula LO, Morsch VM, Martins AF, et al. Effect of mercuric chloride intoxication and dimercaprol treatment on delta-aminolevulinate dehydratase from brain, liver and kidney of adult mice. Pharmacol Toxicol 1996;79:136–43.ArticlePubMed
- 8. Tanaka-Kagawa T, Suzuki M, Naganuma A, Yamanaka N, Imura N. Strain difference in sensitivity of mice to renal toxicity of inorganic mercury. J Pharmacol Exp Ther 1998;285:335–41.PubMed
- 9. Orr SE, Bridges CC. Chronic kidney disease and exposure to nephrotoxic metals. Int J Mol Sci 2017;18:1039.ArticlePubMedPMC
- 10. Jalili C, Kazemi M, Cheng H, Mohammadi H, Babaei A, Taheri E, et al. Associations between exposure to heavy metals and the risk of chronic kidney disease: a systematic review and meta-analysis. Crit Rev Toxicol 2021;51:165–82.ArticlePubMed
- 11. Afrifa J, Essien-Baidoo S, Ephraim RK, Nkrumah D, Dankyira DO. Reduced egfr, elevated urine protein and low level of personal protective equipment compliance among artisanal small scale gold miners at Bibiani-Ghana: a cross-sectional study. BMC Public Health 2017;17:601.ArticlePubMedPMCPDF
- 12. Moon CS, Lee CK, Hong YS, Ikeda M. Higher cadmium burden in coastal areas than in inland areas in Korea: implications for seafood intake. Asia Pac J Clin Nutr 2014;23:219–24.ArticlePubMed
- 13. You CH, Kim BG, Jo EM, Kim GY, Yu BC, Hong MG, et al. The relationship between the fish consumption and blood total/methyl-mercury concentration of costal area in Korea. Neurotoxicology 2012;33:676–82.ArticlePubMed
- 14. U.S. Environmental Protection Agency (EPA). Method 7473 (SW-846): Mercury in Solids and Solutions by Thermal Decomposition, Amalgamation, and Atomic Absorption Spectrophotometry. EPA; 2000.
- 15. Seo JW, Hong YS, Kim BG. Assessment of lead and mercury exposure levels in the general population of Korea using integrated national biomonitoring data. Int J Environ Res Public Health 2021;18:6932.ArticlePubMedPMC
- 16. Ministry of Health & Welfare. Clinical Laboratory Test for the Seventh Korea National Health and Nutrition Examination Survey (2016-2018). Ministry of Health & Welfare; 2019.
- 17. Mahaffey KR, Clickner RP, Bodurow CC. Blood organic mercury and dietary mercury intake: National Health and Nutrition Examination Survey, 1999 and 2000. Environ Health Perspect 2004;112:562–70.ArticlePubMedPMC
- 18. McKelvey W, Gwynn RC, Jeffery N, Kass D, Thorpe LE, Garg RK, et al. A biomonitoring study of lead, cadmium, and mercury in the blood of New York city adults. Environ Health Perspect 2007;115:1435–41.ArticlePubMedPMC
- 19. Schober SE, Sinks TH, Jones RL, Bolger PM, McDowell M, Osterloh J, et al. Blood mercury levels in US children and women of childbearing age, 1999-2000. JAMA 2003;289:1667–74.ArticlePubMed
- 20. Barchiesi F, Branciari R, Latini M, Roila R, Lediani G, Filippini G, et al. Heavy metals contamination in shellfish: benefit-risk evaluation in Central Italy. Foods 2020;9:1720.ArticlePubMedPMC
- 21. Mok JS, Kwon JY, Son KT, Choi WS, Kim PH, Lee TS, et al. Distribution of heavy metals in internal organs and tissues of Korean molluscan shellfish and potential risk to human health. J Environ Biol 2015;36:1161–7.PubMed
- 22. Yang H, Shu Y. Cadmium transporters in the kidney and cadmium-induced nephrotoxicity. Int J Mol Sci 2015;16:1484–94.ArticlePubMedPMC
- 23. Nordberg M, Jin T, Nordberg GF. Cadmium, metallothionein and renal tubular toxicity. IARC Sci Publ 1992;(118):293–7.
- 24. Thevenod F. Nephrotoxicity and the proximal tubule: insights from cadmium. Nephron Physiol 2003;93:87–93.Article
- 25. Bridges CC, Joshee L, Zalups RK. Multidrug resistance proteins and the renal elimination of inorganic mercury mediated by 2,3-dimercaptopropane-1-sulfonic acid and meso-2,3-dimercaptosuccinic acid. J Pharmacol Exp Ther 2008;324:383–90.ArticlePubMedPMC
- 26. Gritzka TL, Trump BF. Renal tubular lesions caused by mercuric chloride. Electron microscopic observations: degeneration of the pars recta. Am J Pathol 1968;52:1225–77.PubMedPMC
- 27. Chapter 1: Definition and classification of CKD. Kidney Int Suppl (2011) 2013;3:19–62.ArticlePubMedPMC
- 28. Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, et al. Slower decline of glomerular filtration rate in the Japanese general population: a longitudinal 10-year follow-up study. Hypertens Res 2008;31:433–41.ArticlePubMed
- 29. Hemmelgarn BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, et al. Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int 2006;69:2155–61.ArticlePubMed
- 30. Cherian MG, Hursh JB, Clarkson TW, Allen J. Radioactive mercury distribution in biological fluids and excretion in human subjects after inhalation of mercury vapor. Arch Environ Health 1978;33:109–14.ArticlePubMed
References
Figure & Data
References
Citations

- Impact of dietary education on blood cadmium and mercury levels in chronic kidney disease: a path to renal health improvement
Ho Sik Shin
Kosin Medical Journal.2023; 38(2): 73. CrossRef

 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite

