Articles
- Page Path
- HOME > Kosin Med J > Volume 38(4); 2023 > Article
-
Case report
Selective adjuvant radiation therapy for distant lymph node metastasis in patients with stage 4B epithelial ovarian cancer: a case series -
Eun Taeg Kim1,2
 , Seung Yeon Oh1
, Seung Yeon Oh1 , Sun Young Ma3,4
, Sun Young Ma3,4 , Tae Hwa Lee1,2
, Tae Hwa Lee1,2 , Won Gyu Kim1
, Won Gyu Kim1
-
Kosin Medical Journal 2023;38(4):293-299.
DOI: https://doi.org/10.7180/kmj.23.146
Published online: December 20, 2023
1Department of Obstetrics and Gynecology, Kosin University Gospel Hospital, Busan, Korea
2Department of Obstetrics and Gynecology, Kosin University College of Medicine, Busan, Korea
3Department of Radiology, Kosin University Gospel Hospital, Busan, Korea
4Department of Radiology, Kosin University College of Medicine, Busan, Korea
- Corresponding Author: Won Gyu Kim, MD, PhD Department of Obstetrics and Gynecology, Kosin University Gospel Hospital, 262 Gamcheon-ro, Seo-gu, Busan 49267, Korea Tel: +82-51-990-6227 Fax: +82-51-244-6939 E-mail: kimwongyu203@naver.com
Copyright © 2023 Kosin University College of Medicine.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 896 Views
- 20 Download
Abstract
- Although the efficacy of surgery followed by taxane- and platinum-based systemic chemotherapy has been clearly demonstrated in the standard first-line treatment of epithelial ovarian cancer, the role of radiation therapy for distant lymph node metastasis in patients with epithelial ovarian cancer is not well-established due to a lack of reported studies. We identified four patients who underwent selective adjuvant radiation therapy for neck and para-aortic lymph node lesions after primary debulking surgery between 2020 and 2022, followed by platinum-based chemotherapy for stage 4B high-grade serous ovarian cancer. Through a retrospective review of medical records, we analyzed patient clinicopathologic features, treatment course, and imaging findings. The median age was 49.25 years (range, 46–54 years). All patients had the International Federation of Gynecology and Obstetrics stage 4B disease. Following primary debulking surgery, all patients received weekly paclitaxel-carboplatin chemotherapy and maintenance treatment with poly(ADP-ribose) polymerase (PARP) inhibitors. All patients received selective adjuvant radiation therapy for neck and para-aortic lymph node metastasis before PARP inhibitor maintenance. The median follow-up time was 36.75 months (range, 19–45 months). All patients achieved a complete response. None of the patients experienced disease recurrence or died during the follow-up period. The management of distant lymph node metastasis in patients with epithelial ovarian cancer remains a matter of debate. Selective adjuvant radiation therapy in first-line treatment for ovarian cancer appears to be a feasible approach with maintenance therapy for stage 4B epithelial ovarian cancer.
- Standard first-line treatment for epithelial ovarian cancer (EOC) consists of primary debulking surgery (PDS), adjuvant platinum-based combination chemotherapy, and individualized maintenance approaches [1]. PDS plays a key role in the treatment of EOC. Maximal cytoreduction was one of the most reliable indicators of survival outcomes among patients with stage III or stage IV ovarian cancer in a meta-analysis [2].
- Recent research from a randomized controlled trial (the LION study) found that systematic lymphadenectomy was not beneficial for patients with advanced EOC with clinically negative lymph nodes who underwent macroscopically complete resection [3]. However, other studies have reported potential survival advantages of retroperitoneal lymphadenectomy for patients with advanced high-grade serous carcinoma (HGSC) after macroscopically complete tumor resection [4]. The lymphadenectomy group in the LION study indicated that systematic lymphadenectomy was associated with a substantial increase in morbidity. In addition, distal lymph node metastasis resection of advanced ovarian cancer requires additional surgical time.
- The effectiveness of radiation therapy in treating distant lymph node metastases from other gynecologic malignancies has been thoroughly evaluated [5,6]. In EOC, it remains unclear whether radiation therapy to metastatic distant lymph nodes contributes to subsequent increases in the survival rate. We retrospectively reviewed four HGSC patients who underwent adjuvant radiation therapy after PDS and platinum-based combination chemotherapy to determine a feasible approach for distant lymph node metastasis in EOC.
Introduction
- Ethical statements: The Institutional Review Board of Kosin University Gospel Hospital reviewed and approved this report (No 2023-10-002). Informed consent was waived.
- 1. General information
- Between January 2020 and February 2022, we identified four patients diagnosed with HGSC who underwent selective adjuvant radiation therapy at neck and para-aortic lymph node lesions after PDS followed by platinum-based chemotherapy (weekly paclitaxel and tri-weekly carboplatin). PDS was performed by a single gynecologic oncologist. The extent of the surgery included bilateral salpingo-oophorectomy, hysterectomy, omentectomy, bilateral pelvic lymph node dissection, and removal of any visible tumors from the pelvic and low abdominal areas. Except for the subclavian lymph nodes and the para-aortic lymph nodes located above the level of the inferior mesenteric artery, the patients underwent maximal cytoreduction surgery (residual tumor of <1 cm). The para-aortic lymph node lesion firmly attached to the major vessels, such as the aorta and vena cava, was considered inoperable. In such cases, we performed a biopsy of the lateral lesion through maximal effort of cytoreduction. Blood Sanger sequencing was immediately performed after diagnosis by histology. The patients' clinical aspects and imaging findings were analyzed retrospectively by assessing their medical records. Clinical details, age at diagnosis, the International Federation of Gynecology and Obstetrics (FIGO) stage, histology, preoperative tumor markers, operative findings, adjuvant treatment, status of BRCA mutation, follow-up duration, and current status were reviewed.
- 2. Radiation therapy method
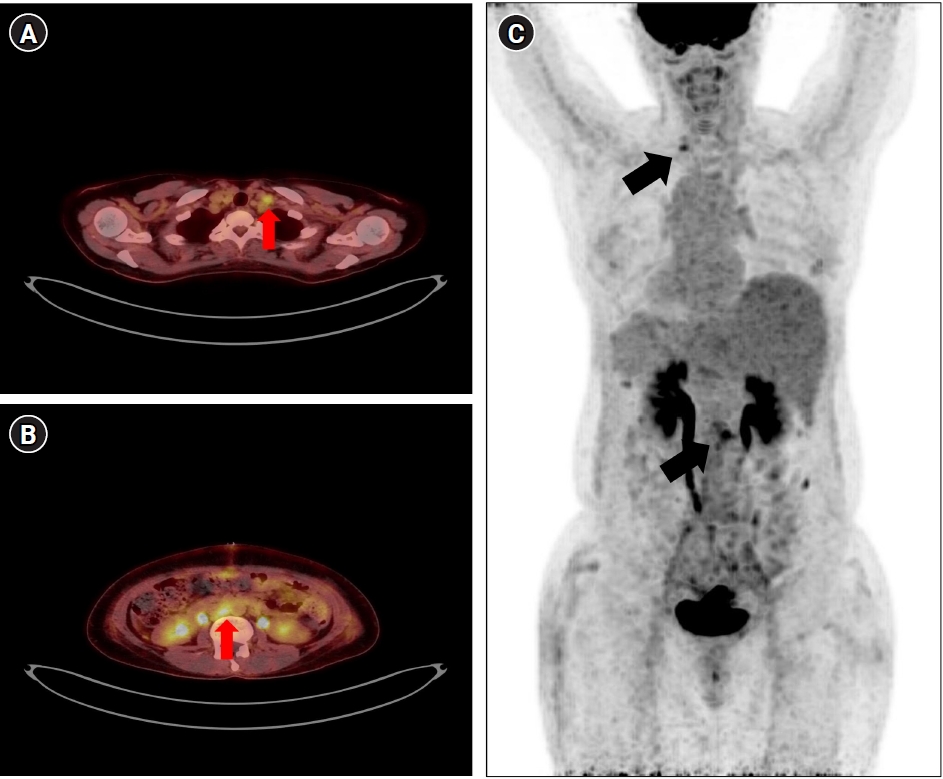
- All patients underwent positron emission tomography-computed tomography (PET-CT) before surgery, and fine needle aspiration biopsy confirmed that the PET-CT showed a supraclavicular lymph node (Fig. 1). Based on the results of the BRCA test, poly(ADP-ribose) polymerase (PARP) inhibitor maintenance was performed after standard treatment of PDS and platinum-based combination chemotherapy. All patients were in complete remission (CR) with no evidence of disease at the beginning of maintenance treatment. Based on the preoperative CT scan, it was determined that radiotherapy would be appropriate for lymph node lesions that exceeded a size of 1 cm and were localized within a limited anatomical region. Conversely, lymph node lesions exhibiting both nodular and diffuse characteristics were decided beyond the scope of radiotherapy, as it was determined that chemotherapy had already covered the lesion within the therapeutic range. This evaluation was conducted by a multidisciplinary team that included a gynecologic oncology radiologist before radiation therapy. Before maintaining the PARP inhibitor, the multidisciplinary team determined the optimal timing for selective adjuvant radiation therapy for the distant metastatic lymph node, which encompassed para-aortic and subclavian lymph node lesions on PET-CT. CT-based three-dimensional treatment planning was performed for all patients. The clinical target volume of radiation therapy was tailored for each patient. For either supraclavicular lymph node or para-aortic lymph node metastasis, the entire lymph node lesion was designated as the clinical target volume. The total radiation dose was 50.4 Gy and was delivered in 28 fractions of 1.8 Gy to each lymph node area.
- 3. Results
- Adjuvant radiation therapy was successfully completed in all patients. The median age was 49.25 years, ranging from 46 to 54 years. All patients had FIGO stage 4B disease. BRCA mutations were identified in two patients (BRCA1 mutation and BRCA2 mutation, respectively). All patients underwent adjuvant radiation therapy for a previous lymph node metastatic lesion during PARP inhibitor maintenance. There were no grade 3, 4, or worse acute adverse events related to radiation therapy. The only radiation-related adverse effect was erythematous pigmentation in one patient (patient 1 in Table 1). The median follow-up time was 36.75 months, ranging from 19 to 45 months. All patients achieved a complete response. None of the patients experienced disease recurrence or died during the follow-up period. Detailed clinicopathological characteristics of the four patients are shown in Table 1.
Case
- The standard treatment of EOC currently involves a multimodal approach that includes PDS, chemotherapy, and tailored maintenance therapies [1]. The extent of lymph node dissection depends on various factors, including the extent of the tumor, the patient's overall health, and the surgical team's decision [4]. The primary goal is maximizing successful treatment chances while minimizing surgical risks.
- An optimal debulking surgery remains the most significant prognostic factor in advanced EOC treatment. Leaving less than 1 cm of residual tumor after debulking surgery is associated with an increased survival advantage in contrast to leaving more than 1 cm of residual tumor [7]. Suboptimal surgery has a negative effect on survival; thus, interval debulking surgery (IDS) after neoadjuvant chemotherapy (NACT) could be an alternative if complete cytoreduction is not possible [8,9]. IDS after NACT and PDS are two surgical approaches used in the management of advanced EOC. While both techniques aim to achieve optimal cytoreduction, they differ in the timing of surgery. IDS is often performed after a course of NACT, which helps to shrink the tumor and decrease tumor burden to decrease surgical complexity and postoperative complications. IDS following NACT is associated with a higher rate of optimal debulking surgery in advanced EOC than in PDS [10]. While NACT can effectively reduce the tumor size, there is a risk of disease progression during chemotherapy, leading to a decrease in the chance of optimal cytoreduction [11]. This risk highlights the importance of careful patient selection for IDS and vigilant monitoring of disease response during NACT. Based on these results, there are no accurate and broadly used indications for NACT. Moreover, if optimal debulking is anticipated, PDS should be performed with preference [12]. Cases in the present study showed distant lymph node metastasis to para-aortic and supraclavicular nodes. In addition, all four cases showed surgical results of minimal residual tumors (residual tumor of <1 cm) except for the distant para-aortic and supraclavicular lymph nodes. Maintaining treatment without complications that can cause discontinuation of standard frontline therapy for ovarian cancer is essential. The excision of extra-pelvic lymph node metastases in advanced ovarian cancer requires a prolonged surgical time and a substantially more complex procedure [13]. Moreover, lymphadenectomy with bulky nodes in advanced ovarian cancer is technically a different procedure than that in early ovarian cancer. Zang et al. [14] reviewed 25 patients with EOC who were initially diagnosed with extra-abdominal metastases. Their study demonstrated that patients with supraclavicular lymph node metastasis had a better prognosis than those with other stage 4 EOC. This clinical perspective indicates that lymphadenectomy in advanced ovarian cancer be performed subsequent to a prolonged and complicated surgical procedure, and it is correlated with high mortality and morbidity [3].
- The optimal approach for managing oligometastatic progression in recurrent ovarian cancer is similarly debatable. There are a few published studies in which various therapeutic strategies were used to manage oligometastatic disease in recurrent ovarian cancer. A study by Palluzzi et al. [15] reviewed the data of 30 patients with ovarian cancer with oligometastatic progression while undergoing maintenance therapy with PARP inhibitors. Ten patients (33%) were treated with surgery, and 20 patients (67%) were treated with stereotactic radiotherapy. In this study, patients with peritoneal recurrences were primarily treated with surgery, while nodal recurrences were treated with stereotactic body irradiation. There were few severe side effects and no difference in survival benefit between the two approaches. Treatment for ovarian cancer is highly individualized. Surgeons are faced with the challenge of balancing performance of optimal cytoreduction and the potential hazards associated with complete removal of all metastatic lymph nodes. Adjuvant radiation therapy after PDS is a beneficial alternative to surgical excision for lesions with high surgical morbidity. Selective adjuvant radiation therapy allows targeted treatment by focusing on involved lymph nodes while sparing uninvolved areas. Based on molecular knowledge, ovarian cancer is radiation-sensitive, and technological advances in radiation treatment for ovarian cancer patients have regained appeal. By avoiding unnecessary surgical interventions, the risk of complications can be reduced [16]. Additionally, concurrent delivery of radiation therapy with maintenance therapy, such as PARP inhibitors, may enhance treatment efficacy by targeting both systemic and loco-regional disease control. However, the current evidence is limited, and patient selection criteria play a crucial role in identifying those most likely to benefit from this modality.
- When a patient presents with metastatic lymph nodes, it is essential to identify the primary metastatic lesions before initiating standard treatment. In the present cases, subsequent chemotherapy was administered to all four patients who had undergone PDS, and the patients achieved CR before maintenance treatment with PARP inhibitor. From the molecular perspective of advanced EOC, even if imaging findings indicate CR, there is a high possibility that residual microscopic lesions remain, necessitating adjuvant treatment [17]. Extra-abdominal lymph node lesions were confirmed by fine needle aspiration biopsy, and intra-abdominal extra-pelvic lymph node lesions were confirmed by intraoperative biopsy. The application of PET-CT imaging at the initial evaluation allows precise identification of the origin of histologically proven metastatic lymph nodes [18].
- Our study had several limitations. First, it was a retrospective, single-center study; this study is subject to biases inherent to this research design, including potential selection and information bias. Second, the number of cases is small. With only four patients in this study, it may not represent the broader population of patients with stage 4B EOC. The absence of a control group of patients who did not undergo selective adjuvant radiation therapy restricts our ability to draw direct causative conclusions from our results. Increasing the size of the sample and expanding the patient cohorts would yield statistically valid outcomes. However, case reports or case series provide a platform for researchers to share their clinical experiences, highlight rare or distinctive manifestations, and convey instructive messages [19]. It underscores the point that even a limited number of cases can have meaningful clinical implications. Third, the median follow-up of less than 4 years might not be sufficient to determine long-term outcomes or potential late complications of radiation therapy. More data and further prospective studies are needed to investigate whether the efficacy and safety of selective adjuvant radiation therapy for distant lymph node metastatic lesions are suitable for the treatment of advanced ovarian cancer.
- In conclusion, the management of distant lymph node metastasis in EOC remains controversial. Selective adjuvant radiation therapy in frontline treatment for ovarian cancer appears feasible, providing targeted treatment and sequential maintenance therapy with PARP inhibitors.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization: ETK, WGK. Data curation: SYO. Fornal analysis: SYO. Validation: SYM, THL. Supervision: WGK, SYM, THL. Visualization: SYM. Writing - original draft: ETK. Writing - review & editing: ETK, WGK.
Article information

FIGO, International Federation of Gynecology and Obstetrics; CA-125, cancer antigen-125; PET-CT, positron emission tomography-computed tomography; TAH, trans abdominal hysterectomy; BSO, bilateral salpingo-oophorectomy; BPLND, bilateral pelvic lymph node dissection; LAR, low anterior resection; Lt., left; Rt., right; SCN, supraclavicular lymph nodes; PAN, para-aortic lymph nodes; CR, complete remission; NED, no evidence of disease.
- 1. Baek MH, Park EY, Ha HI, Park SY, Lim MC, Fotopoulou C, et al. Secondary cytoreductive surgery in platinum-sensitive recurrent ovarian cancer: a meta-analysis. J Clin Oncol 2022;40:1659–70.ArticlePubMed
- 2. Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 2002;20:1248–59.ArticlePubMed
- 3. Harter P, Sehouli J, Lorusso D, Reuss A, Vergote I, Marth C, et al. A randomized trial of lymphadenectomy in patients with advanced ovarian neoplasms. N Engl J Med 2019;380:822–32.ArticlePubMed
- 4. Ikeda Y, Yoshihara M, Tamauchi S, Yokoi A, Yoshikawa N, Kajiyama H. Survival benefits of retroperitoneal lymphadenectomy for optimally-resected advanced ovarian high-grade serous carcinoma: a multi-institutional retrospective study. J Gynecol Oncol 2022;33:e40.ArticlePubMedPMCPDF
- 5. Hata M, Miyagi E, Koike I, Numazaki R, Asai-Sato M, Kasuya T, et al. Radiation therapy for para-aortic lymph node metastasis from uterine cervical cancer. Anticancer Res 2015;35:4849–54.PubMed
- 6. Shaikh T, Churilla TM, Mantia-Smaldone GM, Chu C, Rubin SC, Anderson PR. The role of adjuvant radiation in lymph node positive endometrial adenocarcinoma. Gynecol Oncol 2016;141:434–9.ArticlePubMed
- 7. Chang SJ, Hodeib M, Chang J, Bristow RE. Survival impact of complete cytoreduction to no gross residual disease for advanced-stage ovarian cancer: a meta-analysis. Gynecol Oncol 2013;130:493–8.ArticlePubMed
- 8. Kehoe S, Hook J, Nankivell M, Jayson GC, Kitchener H, Lopes T, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet 2015;386:249–57.ArticlePubMed
- 9. Vergote I, Trope CG, Amant F, Kristensen GB, Ehlen T, Johnson N, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med 2010;363:943–53.ArticlePubMed
- 10. du Bois A, Baert T, Vergote I. Role of neoadjuvant chemotherapy in advanced epithelial ovarian cancer. J Clin Oncol 2019;37:2398–405.ArticlePubMed
- 11. Sato S, Itamochi H. Neoadjuvant chemotherapy in advanced ovarian cancer: latest results and place in therapy. Ther Adv Med Oncol 2014;6:293–304.ArticlePubMedPMCPDF
- 12. Rutten MJ, van de Vrie R, Bruining A, Spijkerboer AM, Mol BW, Kenter GG, et al. Predicting surgical outcome in patients with International Federation of Gynecology and Obstetrics stage III or IV ovarian cancer using computed tomography: a systematic review of prediction models. Int J Gynecol Cancer 2015;25:407–15.PubMed
- 13. Raban O, Peled Y, Krissi H, Goldberg N, Aviram A, Sabah G, et al. The significance of paracardiac lymph-node enlargement in patients with newly diagnosed stage IIIC ovarian cancer. Gynecol Oncol 2015;138:259–62.ArticlePubMed
- 14. Zang RY, Zhang ZY, Cai SM, Tang MQ, Chen J, Li ZT. Epithelial ovarian cancer presenting initially with extraabdominal or intrahepatic metastases: a preliminary report of 25 cases and literature review. Am J Clin Oncol 2000;23:416–9.PubMed
- 15. Palluzzi E, Marchetti C, Cappuccio S, Avesani G, Macchia G, Gambacorta MA, et al. Management of oligometastatic ovarian cancer recurrence during PARP inhibitor maintenance. Int J Gynecol Cancer 2022;32:1164–70.Article
- 16. Macchia G, Titone F, Restaino S, Arcieri M, Pellecchia G, Andreetta C, et al. Is it time to reassess the role of radiotherapy treatment in ovarian cancer? Healthcare (Basel) 2023;11:2413.ArticlePubMedPMC
- 17. Narod S. Can advanced-stage ovarian cancer be cured? Nat Rev Clin Oncol 2016;13:255–61.ArticlePubMedPDF
- 18. Hong L, Qiu H, Mei Z, Zhang H, Liu S, Cao H. Ovarian cancer initially presenting with supra-clavicular lymph node metastasis: a case report. Oncol Lett 2018;16:505–10.ArticlePubMedPMC
- 19. Im SI. How to write case reports in medicine. Kosin Med J 2022;37:102–6.ArticlePDF
References
Figure & Data
References
Citations


 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite