Pathological differences between forceps biopsy specimens and endoscopic resection specimens in early gastric cancer patients
Article information
Abstract
Abstract
Objective:
Endoscopic resection(ER) is effective therapy on EGC and which is treated according to the histological diagnosis of forcep biopsy. But sometimes the histological diagnosis of forcep biopsy and post-ER does not match with each other and it might lead to wrong treatment. The aim of this study is to find the frequency of histologic differences between forcep biopsy and post-ER, and to confirm the characteristics of lesions which make errors.
Methods:
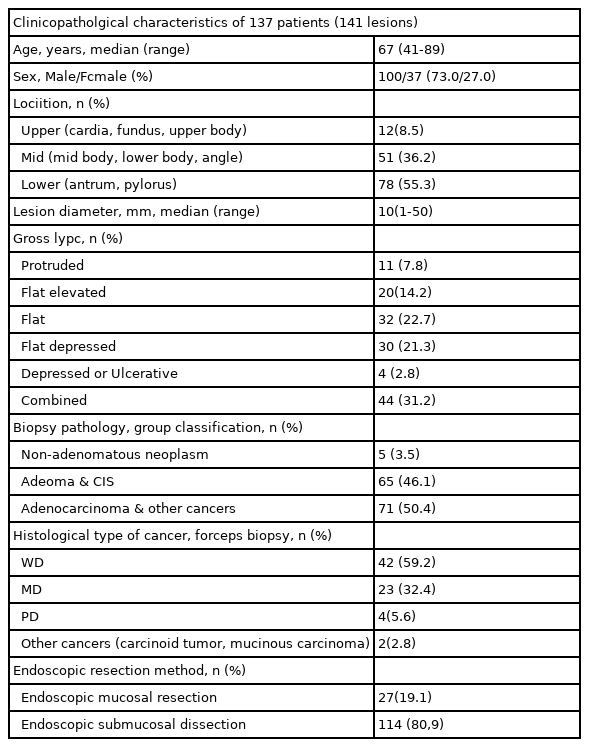
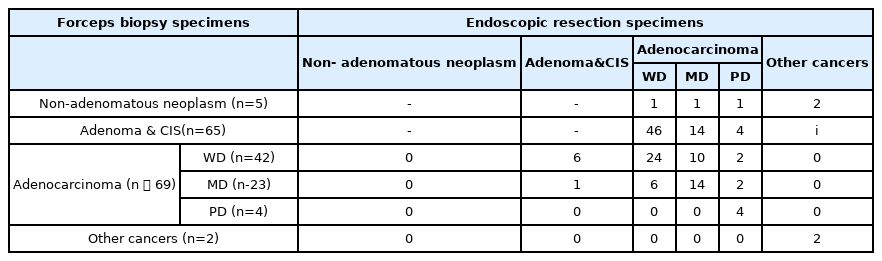
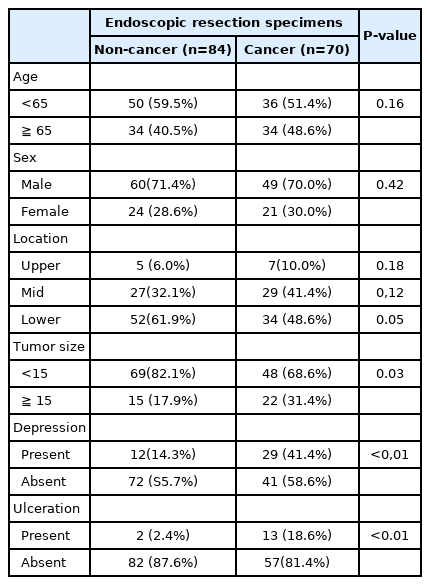
We selected the confirmed cancer cases of 141 patients of 1359 gastric tumor lesions which were treated under the ER in Eulji university hospital from May 2005 to March 2013. They were sorted by the age and sex of patient, location of lesion, present of ulcer and depression to identify the discordance between forcep biopsy and ER. The discordant group was compared with non-cancer-diagnosed controlled group, retrospectively.
Results:
70 cases(5.5%) of 1283 cases of “cancer negative” in forceps biopsy were fo䴸nd to be diagnosed cancer on final diagnosis of cancer by post-ER result. In this discordant group showed characteristics of bigger size that are with more frequently in tumor size D15mm(17.9% vs. 31.4%, p=0.03), have depressed lesion(ᄀ 4.3% vs. 41.4%, p<0.01) and have 䴸lceration(2.4% vs.18.6%, p<0.01) than that of 84 control gro䴸p not diagnosed cancer.
Conclusions:
In cases of tumor with size D15mm, presented with depressed lesion and ulceration, we should consider combined cancer, even the result of forcep biopsy was negative. Therefore, more careful and accurate resection should be taken with characters listed above.
Analysis of the Predictable Factors of Pathological Differences between Non-cancer and Cancer after Endoscopic Resection