Surgical management of giant adrenal myelolipoma using a modified Makuuchi incision: a case report
Article information
Abstract
Giant adrenal myelolipomas are rare, benign, and hormonally inactive tumors. We present the case of a 53-year-old man with a 19-cm retroperitoneal mass, initially suspected to be a retroperitoneal liposarcoma, angiomyolipoma, or adrenal myelolipoma. After conducting endocrine assessments, which were within normal ranges, we decided to perform surgical excision using a modified Makuuchi incision. The tumor was successfully removed, and the final pathological examination confirmed the diagnosis of adrenal myelolipoma. The patient was discharged with no complications and remained without disease recurrence or distant metastasis as of 1 year postoperatively. In conclusion, giant myelolipomas are rare and cause symptoms owing to their large size. Surgical removal is recommended for large or symptomatic myelolipomas. The modified Makuuchi incision allows efficient and safe tumor removal in open surgery for giant myelolipomas.
Introduction
Adrenal myelolipomas are rare, benign, and hormonally inactive tumors. They are the second most common benign tumors of the adrenal glands, after adrenocortical adenoma [1]. However, giant adrenal myelolipomas >10 cm are rarely reported [2,3]. These tumors are composed of mature adipose tissues and hematopoietic elements. They can be confused with retroperitoneal liposarcomas on computed tomography (CT). In our case, we present a case of surgical management of giant adrenal myelolipoma using a modified Makuuchi incision with approval from the institutional ethics committee [4,5].
Case
Ethical statements: This report was approved by the Institutional Ethics Committee of Pusan National University Hospital (2306-015-128). Informed consent was waived because the retrospective design of the study.
A 53-year-old man presented to the clinic with a 19 cm sized, well-defined, heterogeneous fatty mass in the right retroperitoneum, found incidentally on CT. He was obese (176 cm, 102 kg, body mass index 32.92 kg/m2) and had a history of hypertension. Owing to its large volume, the tumor abutted the liver, right kidney, second duodenal portion, and inferior vena cava. However, there was no evidence of distant metastasis or significantly enlarged lymph nodes. The tumor was suggestive of retroperitoneal liposarcoma, angiomyolipoma, or adrenal myelolipoma (Fig. 1). The endocrine assessment included serum cortisol, catecholamines, urinary vanillylmandelic acid, 17-ketosteroids, and testosterone. All parameters were within the normal ranges.
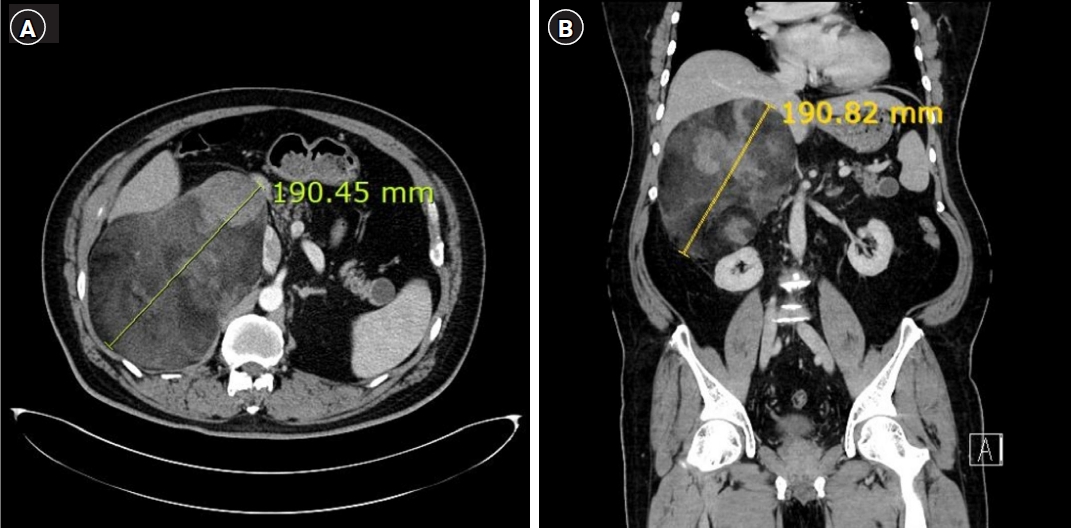
Abdominal computed tomography performed as part of the preoperative evaluation, showing an axial image (A) and a coronal image (B) of the right retroperitoneal mass.
We decided to do a surgical excision with modified Makuuchi (MM) incision (reversed L-shaped incision) with the patient in the supine position (Fig. 2). The tumor was excised with careful attention to the surrounding organs and blood vessels. The operation time was 200 minutes; no damage to surrounding organs occurred during the operation. The postoperative estimated blood loss volume was 500 mL, but there were no major intraoperative vessel injuries. The surgical drain was removed on postoperative day 7, and no complications occurred in the postoperative period. The patient was discharged from the hospital on the 10th postoperative day. Final pathological assessment led to the diagnosis of adrenal myelolipoma (23.8×19.3×9.5 cm, 1.94 kg) (Figs. 3, 4). The histopathology report showed that the tumor comprised mature and variable-sized adipocytes combined with hematopoietic elements from adrenal gland tissue in the peripheral region.
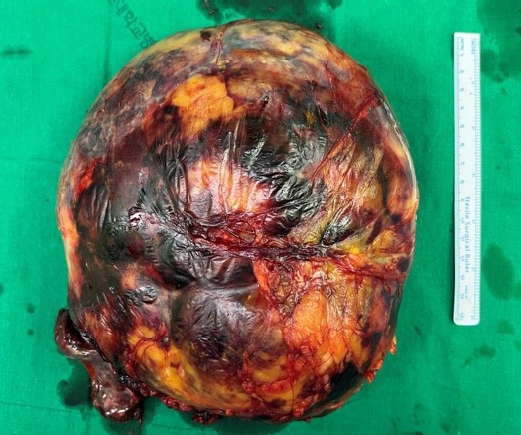
Postoperative macroscopic findings, showing a massive ovoid encapsulated mass (23.8×19.3×9.5 cm, 1.94 kg).

Pathologic slides of the myelolipoma specimen, which is composed of adipose tissue and myeloid tissue (hematoxylin and eosin stain, x200).
The patient was discharged after the incision wound healed on the 10th day after surgery. The patient remained stable 1 year postoperatively without evidence of disease recurrence or distant metastasis.
Discussion
Adrenal myelolipoma is a benign adrenal neoplasm composed of lipoid and myeloid tissue. While its prevalence in the general population is low at 0.2%, it is a relatively common finding in primary adrenal tumors, accounting for 6% to 16% of cases, making it the second most common cause of adrenocortical adenomas [6]. Typically, this condition is diagnosed in adults, with a median age of onset between 55 and 65 years, and it affects both sexes equally [1]. While most myelolipomas are asymptomatic, giant myelolipomas are a rare occurrence that can lead to various symptoms due to their size. In severe cases, these symptoms may include dragging abdominal pain, abdominal mass, compression of adjacent organs, or acute intratumoral or retroperitoneal hemorrhage [7].
However, the exact pathogenesis of myelolipomas remains unclear. The most accepted hypothesis is that in response to stimuli, such as inflammation, infection, chronological stress, or necrosis, the reticuloendothelial cells of the blood vessels within the adrenal gland undergo metaplasia resulting in myelolipoma. Evidence supporting this hypothesis includes the fact that myelolipomas are usually diagnosed after middle age. Furthermore, myelolipoma is frequently associated with conditions such as obesity, hypertension, hyperlipidemia, and diabetes, which increase the secretion of the stress hormone cortisol [8,9].
Myelolipoma can be diagnosed using characteristic imaging findings and evaluation of hormonal secretory function. It appears as a heterogeneous mass on CT or magnetic resonance imaging, usually round or oval in shape, with macroscopic fatty tissue inside [1,7] The ratio of fat tissue is highly variable among patients. Myelolipomas are known to be non-functional, but there is controversy with respect to performing hormonal testing [10]. The differential diagnoses of myelolipoma include adrenocortical adenoma, adrenocortical carcinoma, retroperitoneal liposarcoma, exophytic renal angiomyolipoma, and adrenal lipoma [7] and larger tumors are often misinterpreted on radiographic imaging [11,12]. However, biopsies are not recommended because they can lead to bleeding, rupture, or life-threatening shock [2]. Typically, myelolipomas are asymptomatic; therefore, they are often discovered incidentally when they are large. Giant adrenal myelolipomas are usually >10 cm in diameter, and some researchers have suggested that true giant adrenal myelolipomas are >1.5 kg in weight [8].
Myelolipomas are usually removed surgically. Surgery is recommended for larger tumors due to the risk of bleeding and hematoma with spontaneous rupture. The size threshold varies by institution and researcher but is usually between 4 cm and 7 cm, and surgery is recommended for larger sizes [8].
A giant adrenal mass >12 cm in diameter indicates open surgery, especially if the histologic diagnosis of giant myelolipoma is uncertain and malignancy cannot be completely excluded [13]. The choice of open surgical incision for giant myelolipomas may differ depending on the size of the tumor and the surgeon's preference. Most urologists are familiar with the flank, subcostal, chevron, thoracoabdominal, and midline incisions. However, several studies have introduced the MM incision as a game-changer that can overcome the disadvantages of existing incision methods. In 1993, Makuuchi described the Makuuchi incision as a midline incision from the xiphoid to 5 cm above the umbilicus and a second incision to the ninth intercostal area to create a J-shaped curve [14]. Later, Chang modified it by placing a midline incision from the xiphoid process to the umbilicus and a horizontal incision to create a reverse L shape (Fig. 2) [15]. Since then, some surgeons have successfully removed kidney tumors >20 cm and adrenal tumors >30 cm using MM incisions [16,17].
This study introduced the etiologic background and clinical characteristics of this relatively rare adrenal myelolipoma, and presented that when it is found to be a giant adrenal myelolipoma larger than 10 cm, it can be surgically removed successfully using an MM incision. Since this approach for giant adrenal mass has yet to be reported in the urologic field, this study may have clinical significance in introducing it.
In conclusion, adrenal myelolipoma is an asymptomatic, non-functional adrenal mass that is rarely diagnosed incidentally as a giant myelolipoma. It has heterogeneous imaging characteristics, with adipose tissue inside, and should be carefully differentiated from tumors of adrenal origin. Giant myelolipomas require surgical treatment, and given their large diameter and potential for malignancy, open surgery may be an option. The MM incision approach allows efficient and safe tumor removal in open surgery for giant myelolipomas.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: BJK. Data curation: BJK. Investigation: BJK. Methodology: KHK. Supervision: HKH. Visualization: SHK, KJ. Writing - original draft: BJK, . Writing - review & editing: KHK. Approval of final manuscript: all authors.

