Scrub typhus infection in a kidney transplant recipient: a case report
Article information
Abstract
Scrub typhus is a febrile disease that is endemic to Asia and the Pacific region. Its clinical manifestations include fever, myalgia, lymphadenopathy, and a characteristic eschar. The main manifestations of this disease are difficult to differentiate from those of other febrile illnesses; thus, a careful clinical examination and a high index of suspicion are crucial for an early diagnosis. Our case involved a 55-year-old female renal transplant recipient who presented with fever and sore throat in November. Her clinical symptoms did not improve after oral amoxicillin/clavulanate administration for 7 days, after which proteinuria and acute kidney injury were identified. After hospitalization, an eschar was found and immunoglobulin M antibodies against Orientia tsutsugamushi were detected by indirect immunofluorescence. She received oral doxycycline for 7 days and showed improvement in renal function and proteinuria. This is the first case report of scrub typhus infection in a kidney transplant patient in Korea. It is meaningful to report that the renal abnormalities associated with scrub typhus improved in a renal transplant patient through treatment of the disease. This case highlights the importance of examining the social history and symptoms of patients suspected of having scrub typhus in endemic areas. Early diagnosis and treatment are crucial in kidney transplant patients to preserve graft function and prevent fatal complications.
Introduction
Scrub typhus is an acute febrile illness caused by Orientia tsutsugamushi. It is transmitted by the bites of larval Leptotrombidium mites with O. tsutsugamushi [1]. Scrub typhus is endemic to rural areas of Asia and the Pacific region. It is also the most common rickettsial disease in autumn in Korea and occurs nationwide [2]. Clinical findings include fever, myalgia, skin lesions (especially typical eschar), and lymphadenopathy. The disease is usually mild and self-resolving but can occasionally result in severe complications such as interstitial pneumonia, acute kidney injury, multi-organ failure, and death [3]. Renal involvement in scrub typhus ranges from isolated urinary abnormalities to fatal acute kidney injury [4]. As the main manifestations of this disease are difficult to distinguish from other febrile diseases, it is difficult to make an early diagnosis. Eschar is the crucial clue for the diagnosis of scrub typhus, and its overall prevalence ranges from 32.8% to 78.7%. The distribution of eschar is highest in the inguinal area, followed by the anterior area and lower extremities [5]. Because eschar is small and located in moist areas where the skin overlaps, it can be detected through close physical examination. We report the case of a renal transplant recipient with scrub typhus infection who received a delayed diagnosis.
Case
Ethical statement: This study was exempt from review by the Institutional Review Board of Asan Medical Center (IRB No. 2023-0172). Written informed consent was obtained from the patient to participate in the study.
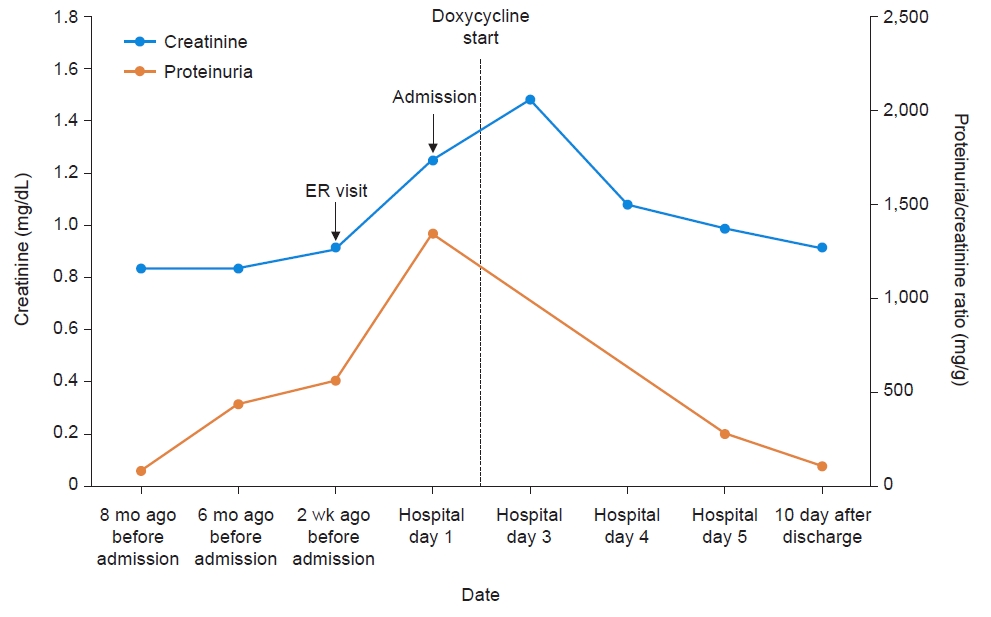
A 55-year-old woman, a renal transplant recipient, visited the outpatient clinic of a tertiary hospital and was referred to the emergency department due to fever and sore throat in November. She had undergone a living donor kidney transplant 2 years prior, did not have any rejection, and was on triple immunosuppressant therapy (tacrolimus 6 mg/day, mycophenolate mofetil 1,000 mg/day, and methylprednisolone 4 mg/day). Two weeks prior, she visited the outpatient clinic on a regular schedule and complained of general weakness and breast pain near the axillary area without fever. One week prior, she visited the emergency room of our hospital because of sore throat and was prescribed oral amoxicillin/clavulanate for 7 days. On the day of admission to the outpatient clinic, despite taking oral antibiotics, fever and sore throat persisted, and laboratory tests showed decreased renal function and proteinuria. She was admitted to our hospital for further examination, mycophenolate mofetil was discontinued, and the dose of methylprednisolone was increased to 10 mg/day. At the time of admission, her vital signs were as follows: blood pressure, 121/80 mmHg; pulse rate, 105 beats/min; body temperature, 37.7 °C; and respiratory rate, 18 breaths/min. The patient was alert. Physical examination revealed tonsillar hypertrophy and redness. An eschar, characteristic of scrub typhus, was observed in the right breast near the axillary area (Fig. 1). Examination of the cardiovascular, respiratory, and abdominal systems revealed normal results. Complete blood cell counts were as follows: white blood cell count, 9,300/mm3 (neutrophil-dominant, 77.9%); hemoglobin, 12.1 g/dL; and platelet count, 170,000/mm3. The biochemistry results were as follows: C-reactive protein level, 10.87 mg/dL; blood urea nitrogen level, 19 mg/dL; creatinine level, 1.25 mg/dL; total protein level, 7.0 g/dL; albumin level, 2.7 g/dL; aspartate transaminase level, 74 IU/L; alanine aminotransferase level, 49 IU/L; uric acid level, 4.2 mg/dL; and lactate dehydrogenase level, 570 IU/L. Microscopic urinalysis showed albumin 1+, occult blood traces, and red blood cells 0-2/high-power field. The urinary creatinine to protein ratio was 1,345.6 mg/g. The results of the anti-human immunodeficiency virus antibody, hepatitis B virus surface antigen, anti-hepatitis B virus surface antibody, and anti-hepatitis C virus antibody tests were negative. The patient lived in a suburban area and had a history of working in gardens. Based on the social history, seasonal factors (November), fever, elevated liver enzyme levels, and typical eschar, serological tests were performed to discriminate between scrub typhus and other febrile diseases. While waiting for the serological test results, rapid diagnostic tests for leptospirosis, scrub typhus, and hemorrhagic fever with renal syndrome were performed. Immunoglobulin (Ig)M antibodies against O. tsutsugamushi were positive; IgG antibodies were weakly positive; and all other tests were negative. Based on these findings, oral doxycycline was immediately administered. As decreased renal function and proteinuria were observed in a renal transplant recipient, renal ultrasonography, cytomegalovirus, BK virus polymerase chain reaction (PCR) tests, and donor-specific antibody (DSA) tests were performed. To discriminate between other viral infections, multiple viral PCR tests were performed for adenovirus, parainfluenza virus, rhinovirus, influenza virus, respiratory syncytial virus, metapneumovirus, enterovirus, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Fever and inflammatory marker levels improved within 48 hours, and renal function and proteinuria improved within 72 hours (Fig. 2). On the third day of hospitalization, the results of an indirect immunofluorescent antibody (IFA) assay were positive for antibodies for O. tsutsugamushi. DSA, cytomegalovirus, and BK PCR results were negative, and renal ultrasonography showed no structural abnormalities. The results of multiple viral PCR tests, including SARS-CoV-2 PCR, were negative. The patient was discharged after 6 days, and her renal function and proteinuria improved to the normal range in an outpatient examination performed 10 days after discharge. The patient maintained normal renal graft function.
Discussion
The clinical features of scrub typhus are similar to those of febrile diseases. Thus, it is important to identify eschar as a pathognomonic sign of scrub typhus. At the site of a tick bite, eschar is formed with a diameter of 5 to 20 mm, covered with a black scab in the middle [2,3]. Although eschar is normally painless, patients often complain of pain due to enlarged lymph nodes around the eschar [2]. Therefore, lymphadenopathy may help locate the eschar if it is small or if it is located in skin overlaps. Our patient presented with breast pain near the axilla, and an eschar was detected on the anterior chest. She complained of breast pain at the outpatient clinic; however, we did not find an eschar at that time. This case highlights the importance of careful physical examinations in outpatient clinical settings.
According to the data from the Korea Disease Control and Prevention Agency, the fatality rate of scrub typhus is as high as 0.2% [6]. Therefore, early diagnosis and appropriate treatment are critical during the epidemic season. Among serological diagnostic tests, the IFA test with high sensitivity and specificity is the gold standard for diagnosing scrub typhus [2]. However, because the IFA test requires some time for diagnosis, a rapid diagnostic test can be helpful for quick diagnosis [7]. In our case, we used a rapid diagnostic test for the early detection of scrub typhus infection. Our patient received antibiotics immediately after the rapid diagnostic test, and there were no sequelae.
The patient presented with proteinuria and decreased renal function upon admission. Proteinuria and hematuria may occur in 10% to 20% of patients with scrub typhus, and acute renal failure has been reported in 8% to 40% of those patients [8-10]. End-stage renal disease is rarely caused by scrub typhus and requires maintenance hemodialysis, and only one case has been reported in Korea [11]. In most patients, acute renal failure due to scrub typhus is reversible with appropriate antibiotic therapy. Our patient was a renal transplant recipient who received triple immunosuppressant therapy, and her highest creatinine level was 1.48 mg/dL during hospitalization. However, after treatment for scrub typhus, renal function and proteinuria recovered to the normal range in the general population.
Reports of scrub typhus infections in renal transplant recipients are rare; however, there has been a case of scrub typhus meningitis in a kidney transplant recipient in India. The patient presented with fever, severe headache, acute renal failure, and proteinuria. An eschar was found on the patient’s back, and IgM antibodies against O. tsutsugamushi were positive. She was administered antibiotics and discharged with normal graft function [12]. No case of scrub typhus in a renal transplant patient has been reported in Korea yet; however, in actual clinical practice, it is thought that such cases may have occurred. In India, there has been a recent report of co-infection with coronavirus disease 2019 (COVID-19) and scrub typhus [13]. Considering the ongoing COVID-19 pandemic, it is necessary to differentiate febrile illnesses based on clinical symptoms and epidemiological factors.
Because kidney transplant recipients are immunocompromised, appropriate tests should be performed for general and opportunistic infections if signs of infection are revealed. It is important to assess the social history and symptoms of scrub typhus during the epidemic season. Early diagnosis and proper management are essential in kidney transplant patients to preserve renal graft function and prevent fatal complications.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: DL, CHB. Data curation: DL. Formal analysis: DL. Methodology: DL, CHB. Investigation: DL, JJ, JSA. Resources: DL, CHB. Supervision: CHB. Visualization: DL. Writing-original draft: DL. Writing-review & editing: DL, CHB.