Revascularization of immature retinas with retinopathy of prematurity using combination therapy of deferred laser treatment after a single intravitreal bevacizumab injection
Article information
Abstract
Background
This study aimed to observe the extent of retinal vascularization in patients with retinopathy of prematurity (ROP) who underwent deferred laser treatment (LT) after a single intravitreal bevacizumab injection (IVB).
Methods
This study retrospectively evaluated 40 consecutive eyes in 21 infants who received a single IVB or LT. Deferred LT was performed in cases of ROP recurrence after a single IVB. To assess the amount of retinal vascularization between the initial IVB and deferred LT, the cases were divided into three groups based on treatment: single IVB, deferred LT after a single IVB, and prompt LT. The growth and associated complications were compared between groups.
Results
There were 12, 16, and 12 eyes in the single IVB, deferred LT, and prompt LT groups, respectively. Deferred LT was performed at an average of 7.9 weeks after a single IVB. In the single IVB group, retinal vascularization proceeded to zone III, whereas the prompt LT group did not show any growth of vascularization beyond the laser scars. In the deferred LT group, during the window period before LT, retinal vascularization progressed from zone I to zone II posterior and from zone II posterior to zone II anterior, respectively, without further ROP recurrence.
Conclusions
Retinal vascularization progressed during the deferred window period, thereby reducing the area of the retina ablated by LT. A single IVB followed by deferred LT can be an alternative treatment option to prevent ablation of zone I or multiple IVBs.
Introduction
Retinopathy of prematurity (ROP) is a major cause of childhood blindness. As the survival rate of premature infants increases, the number of patients with severe ROP is increasing [1]. Laser treatment (LT) remains the main treatment for ROP. In the early treatment for ROP (ET-ROP) trial, 9.1% of patients had unfavorable structural outcomes [2]. After a large area of the retina is demolished by LT or cryotherapy, the normal retinal vascularization process does not proceed, and high myopia and visual field defect occur as they grow.
Recently, intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) have been developed and widely used for ROP. The injection has several advantages compared to LT, such as its simple and less time-consuming procedure; however, anti-VEGF injection can be complicated by late recurrence and is more likely to require retreatment than LT [3,4]. It can also reduce myopic progression and visual field defects caused by peripheral retinal ablation and allow for the growth of the neurovascular retina into the peripheral area [3-6].
Despite the low recurrence rate, there remains concerned regarding the timing of recurrence and appropriate follow-up period after anti-VEGF intravitreal injection. Since the interval between anti-VEGF injection and recurrence is relatively long and varies from several weeks to months, careful follow-up is required until vascularization extends to the peripheral area to prevent unexpected recurrences [4,7,8]. Although it is widely used in clinical practice, there is no protocol for proper management after anti-VEGF injection. In addition to the long-term follow-up to observe ROP recurrence, another issue is the safety of multiple anti-VEGF injections in preterm infants. A single anti-VEGF injection was found to lower blood VEGF for a minimum of 7 to 8 weeks in a human study [9,10]. Because VEGF is an essential factor for the development of several organs, including the retina and brain, a decrease in blood VEGF levels affects infant growth.
Given the need for long-term follow-up and the risk of systemic side effects caused by multiple anti-VEGF injections, administering more than one anti-VEGF injection may carry increased clinical load and potential dangers. To avoid multiple injections, combination therapy with LT and anti-VEGF injection can be performed [11]. However, LT in zone I ROP can cause refractive errors and constriction of the visual field [12,13]. In such a case, deferred LT after an anti-VEGF injection can be an option to prevent the risks of multiple anti-VEGF injections or prompt LT in zone I [14,15]. Despite these points, to the best of our knowledge, the extent of retinal vascularization during the deferred window period has not been specifically studied. Thus, the present study evaluated the growth of vascularized retina after a single intravitreal bevacizumab injection (IVB) until deferred LT.
Methods
Ethical statements: This protocol was approved by the Institutional Review Board of Kosin University Gospel Hospital (IRB No. KUGH 11-21). The study adhered to the tenets of the Declaration of Helsinki, and the informed consent was waived because this study design is a retrospective chart review.
The medical records of consecutive patients with ROP who received a single IVB or LT at three institutions in Busan, South Korea, between 2009 and 2016 were reviewed. Forty eyes of 21 patients who were followed for at least 6 months after receiving a single IVB or LT treatment were included. The eyes were divided into three groups based on the type of treatment: single IVB, deferred LT after single IVB, and prompt LT. Deferred LT was performed when the disease recurred or new vessels regrown and reached stage 3 after a single IVB. Three researchers from each center participated in the study, and each investigator was able to treat each eye differently in the treatment of each infant. Sex, gestational age, birth weight, postmenstrual age at IVB or LT, follow-up duration, surgical intervention, stage, and zone of ROP were investigated.
Routine fundus examinations for ROP screening were based on the ET-ROP guidelines. It was performed using indirect ophthalmoscopy with scleral depression under local anesthesia by three retinal specialists from each institution [16]. ROP zones and stages were classified according to the guidelines of the Revised International Classification for ROP [17]. The anteroposterior location of the ROP was described by retinal specialists at each center according to the aforementioned guidelines. Zone I was defined as a circle whose radius is twice the distance between the center of the optic disc and center of the macula [17]. For the purpose of this study, we divided zone II into posterior and anterior following the definition used by Mintz-Hittner and Kuffel [18]. Zone II posterior was defined as a circle whose radius is three times the distance between the center of the optic disc and center of the macula. Meanwhile, the zone of disease was determined based on the most posteriorly located neovascularization, regardless of extension. Two ophthalmologists identified the zones and stages based on the same criteria as ROP recurrence.
The principle of treatment was applied according to the ET-ROP guidelines, and the method of treatment was independently selected at the discretion of the doctor at each center [16,17]. Infants with any stage of ROP with plus disease in zone I, stage 3 without plus disease in zone I, stage 2 or 3 with plus disease in zone II, or aggressive posterior ROP underwent treatment. Follow-up examinations were performed once or twice a week after the treatment to confirm ROP regression. In case of recurrent ROP, deferred LT was performed after a single IVB and IVB was performed after prompt LT. Recurrence was defined as the reappearance of the plus disease or development of a new demarcation line or above stages. The deferred window period was defined as the period between the first and second treatments. All LT procedures were performed using a diode laser with an 810-nm wavelength instrument under general anesthesia and applied to the avascular retina up to the ora serrata, with half-burn spacing between the laser spots.
IVB was performed under general anesthesia in the operating room. After preparing the eyelids and conjunctiva with 5% povidone iodine, 0.625 mg (0.025 mL) of bevacizumab (Avastin; Genentech Inc.) was intravitreally injected into the 1.5-mm intravitreal cavity in the nasal cavity or temporal limbus. Injection was performed under a surgical microscope using a 30-gauge needle. After the injection, topical antibiotics were administered.
T-tests for independent means, Mann-Whitney rank-sum test, chi-square test, and Fisher exact test were used for statistical analysis with significance (p<0.05). Means and standard deviations are presented as mean (standard deviation). GraphPad Prism version 6.03. (GraphPad Software. Inc.) was used for data analysis.
Results
1. Demographic characteristics
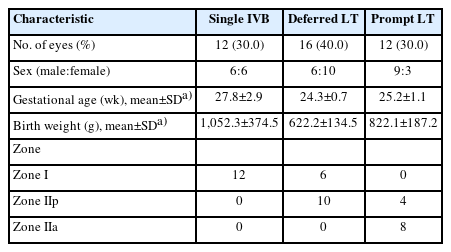
The single IVB, deferred LT after single IVB, and prompt LT groups included 12, 16, and 12 eyes, respectively (Table 1, Fig. 1). The mean birth weights in the single IVB, deferred LT after single IVB, and prompt LT groups were 1,052.3±374.5, 622.2±134.5, and 822.1±187.2 g, respectively (p<0.0001) (Fig. 2A), and the gestational ages of the patients were 27.8±2.9, 24.3±0.7, and 25.2±1.1 weeks, respectively (p<0.0001) (Fig. 2B). The single IVB group had a significantly higher gestational age than the deferred LT group. The recurrence interval between the initial and subsequent treatment was 55.0±11.4 days and 17.0±14.4 days in the deferred LT after single IVB and prompt LT groups, respectively, which showed a significant difference (p=0.0001) (Fig. 2C). ROP recurrence occurred in 10 of 12 patients in the prompt LT group, and all of them underwent IVB. The timing of IVB was 34.7±0.9 weeks in the single IVB group and 32.3±1.7 weeks in the deferred LT group (p=0.0483) (Fig. 2D).

Classification of patients (40 eyes) who received intravitreal bevacizumab injection (IVB) or laser treatment (LT) as an initial treatment for retinopathy of prematurity. The single IVB, deferred LT after single IVB, and prompt LT groups included 12, 16, and 12 eyes, respectively.
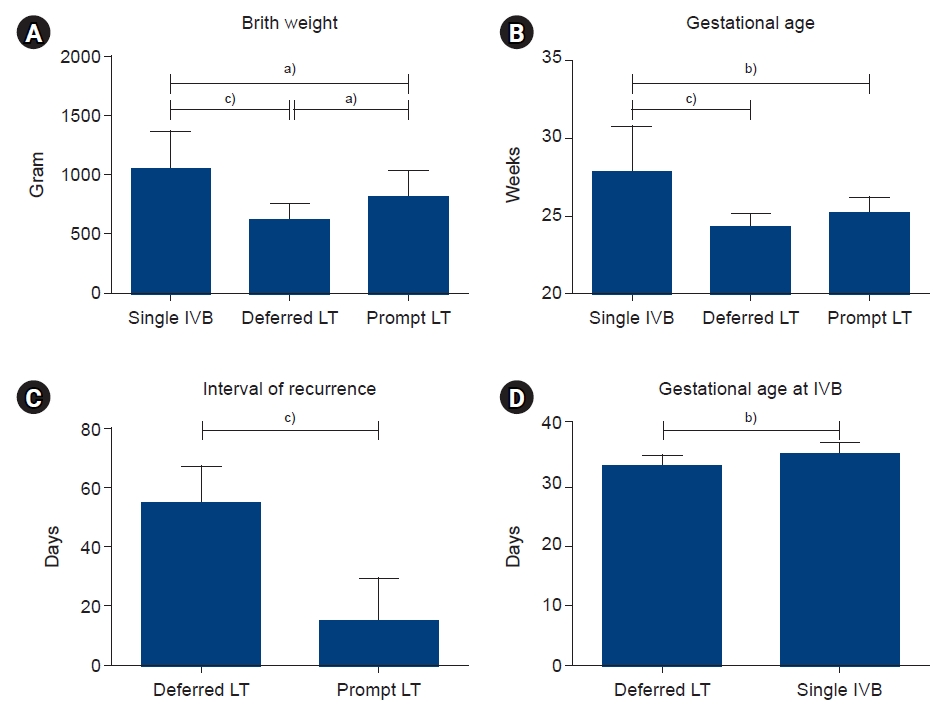
Comparison of birth weight, gestational age, recurrence intervals, and gestational age at the time of intravitreal bevacizumab injection (IVB) in the single IVB, deferred laser treatment (LT) after single IVB, and prompt LT groups. (A) The mean birth weight was significantly different among the groups, and (B) the gestational ages of the single IVB group was significantly higher than that of the other groups (p=0.016). (C) The interval of recurrence between initial treatment and retreatment was significantly longer in the deferred LT after single IVB group than in the prompt LT group (p=0.0001). (D) Gestational age at IVB was significantly more in Single IVB than in deferred LT. Significance: a)p<0.05, b)p<0.005, c)p<0.0001, Kruskal-Wallis test.
2. ROP stage and zone
All 18 eyes with zone I ROP received a single IVB, and 12 eyes had revascularization of the retina and reached zone III without additional treatment (Table 2). The remaining six patients required deferred LT, and retinal vascularization progressed from zone I to zone IIp during the deferred window period. Zone IIp ROP and IIa ROP were noted in 14 and 8 eyes, respectively. Zone IIp ROP was observed in all 14 eyes. Of these, 10 eyes required deferred LT after IVB, and only prompt LT was performed in four eyes. Ten eyes with zone IIp ROP underwent retinal revascularization to zone IIa during the deferred window period, and retinal vascularization did not proceed until the final examination in four eyes with prompt LT only. All eight eyes with zone IIa ROP underwent prompt LT, and retinal vascularization did not progress until the final examination. The average duration from single IVB until deferred LT was 7.9±1.6 weeks. During this deferred window period, retinal vascularization progressed from zone I to zone IIp and from zone IIp to zone IIa.
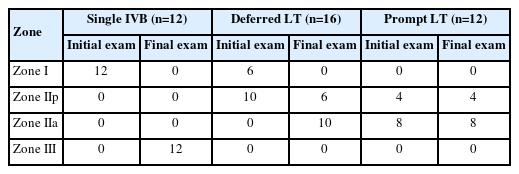
Comparison of the initial and final retinal vascularization in retinopathy of prematurity of the single IVB, deferred LT after single IVB, and prompt LT groups
In all eyes that received bevacizumab injection, the plus sign regressed within 2 to 6 days. In cases where pupillary stiffness and meningeal vessels were observed, neovascularization regressed within 2 to 3 weeks of the injection.
3. Adverse effects
In 40 eyes, short-term adverse effects of IVB within 2 weeks after injection included intraocular pressure elevation (n=1), subconjunctival hemorrhage (n=4), and retinal hemorrhage (n=1). There were no occurrences of infectious endophthalmitis or retinal detachment during the follow-up period, and no systemic complications were observed based on the opinions of the pediatric doctors. All patients showed fixation reflexes and were able to follow the object during the final vision examination. Only one patient in the IVB with deferred LT group showed exotropia due to macular dragging.
Discussion
This study confirmed that when LT was delayed after a single IVB, vascularization of the immature retina was reestablished during this deferred window period and zone I ROP retinal vascularization progressed to zone II and zone IIa ROP to zone IIp. Additionally, deferred LT following a single IVB may minimize the potential systemic side effects of multiple IVBs.
The standard treatment for ROP is LT of the avascular peripheral retina. The ET-ROP trial reported that early LT for high-risk or pre-threshold diseases resulted in better visual and structural outcomes than conventional LT for threshold disease; thus, LT is recommended for the treatment of type I ROP [2]. However, studies have shown that the more the peripheral retina is destroyed, the higher the risk of myopia changes and visual field defects [3,5,9]. Previous studies have reported that the average refractive error of the peripheral retina at 5 to 7 years after LT is –2.3 to –6.7 diopters (D), higher than that in the control group [13,19-22]. Hwang et al. [5] also reported that the myopic change was more severe in zone I ROP than in zone II ROP and that the mean spherical equivalent values were −10.1±10.5 D and −4.7±4.6 D, respectively. These findings were consistent with those of the BEAT ROP (Bevacizumab Eliminates the Angiogenic Threat of ROP) follow-up study [13]. Geloneck et al. [13] showed that, in addition to the myopic shift, visual fields were better preserved with IVB than with LT since IVB could lead to further growth of the peripheral retinal vessels. Considering the benefits of further growth of the vascularized retina, choosing a treatment method that can further revascularize an immature retina will have a significant impact on the patient’s condition in terms of myopic progression and visual field preservation. Additionally, it would be advantageous if the laser could be avoided in zone I when possible. In this study, during the delay period, the location of retinal vascular growth changed from zone I to zone IIp and from zone IIp to zone IIa, avoiding LT in zone I and zone IIp.
Apart from the advantages of IVB, there are concerns regarding the fact that the timing of recurrence after IVB is not constant, the follow-up period is relatively long, and there are systemic side effects. The BEAT ROP study reported that the rates of recurrence of zone I ROP in the IVB and LT groups were 6% and 27%, respectively [4]. Despite the low recurrence rate of IVB, the researchers of the BEAT ROP study had to wait for up to 20 weeks for relapse, and the intervals between IVB and recurrence in the BEAT ROP study were 19.2±8.6 weeks and 14.4±0.8 weeks in zone I and zone II ROP, respectively. Several case reports have described ROP recurrence after IVB. Hoang et al. [7] and Kong et al. [8] reported that ROP recurred 2 months and 11 months after the initial IVB, respectively. The intervals from initial IVB to recurrence were relatively long and variable, which can be affected by multiple factors, such as the systemic condition of the infant, population origin, and type of anti-VEGF agent used [7,8]. In the present study, the interval of ROP recurrence after initial treatment was significantly longer with IVB than with LT. Owing to the recurrence of such unexpected ROP, long-term follow-up is required, but this is impossible in actual clinical settings. For example, a complete examination of the peripheral retina of a baby aged >50 to 60 weeks may require general anesthesia, and there is no clear protocol for this follow-up.
Interestingly, the recurrence interval in this study was shorter than those reported in other studies. In the case of BEAT ROP, after IVB, zone I ROP is 19.2±8.6 weeks and zone II ROP is 14.4±0.8 weeks [4]. The recurrence interval after IVB injection was 8.8±3.9 weeks in the study of Ling et al. [23] and 9.0±7.1 weeks in the study of Tandon et al. [15]. In the study of Hu et al. [24], it was 14.4 weeks. The interval between recurrences after IVB varies considerably between investigators. Although the reason for this difference is unclear, it is assumed that the criteria for retreatment are slightly different among researchers. In this study, we also found that IVB reduced systemic VEGF in infants for nearly 2 months [10]. In that regard, we believe that vitreous VEGF increases again about 8 weeks after IVB and ROP may recur during this period.
To prevent these problems, several clinicians have suggested a combination therapy of IVB and LT [11,25]. Several studies have shown that LT can interfere with the further growth of the ROP vascularized retina [4,19], and deferred LT rather than prompt LT following initial IVB may increase the risk of the progression of retinal vascularization. Recently, studies on deferred LT after IVB have shown good anatomical results with less myopic shift [14,15]. However, no data were presented on the extent to which retinal vascularization progressed while waiting for deferred LT after IVB. The mean durations between IVB and LT were 9.0 and 8.7 weeks, respectively [14,15]. In this study, the average duration was 7.9 weeks; during this period, retinal vascularization resumed, developing zone I into zone IIp and zone IIp into zone IIa. Deferred LT was performed when the plus sign recurred or new vessels regressed after a single IVB regrown and reached stage 3 in this study. However, if the drug used for intraocular injection was not bevacizumab, different results would be expected owing to the different vitreous body clearance rates.
If IVB is performed multiple times, it is possible that vascularization of the retina will progress to zone III; however, prior to this, systemic side effects of multiple IVBs must be considered. Several studies have shown that, from day 1, a proportional amount of IVB is absorbed systemically and can decrease VEGF levels in the blood for up to 7–8 weeks [9,10,26,27]. Systemic VEGF plays an important role in angiogenesis and development of various vital organs in infants [28]. Studies on the effects of systemic VEGF inhibitors in mice have shown the loss of fenestration in organs secondary to VEGF suppression, such as the pancreatic islets, thyroid, adrenal cortex, pituitary, villi of the small intestine, kidney, and choroid plexus [29,30]. In particular, patients with zone I ROP that require IVB are more likely to be affected by systemic side effects due to decreased maturity. In this study, infants who received deferred LT following IVB had a lower average gestational age than those who received a single IVB.
Despite these findings, this study had several limitations. First, it was a multicenter, retrospective study, and there were no randomized controls. This can lead to selection bias. The follow-up period was approximately 6 months, which was relatively short. First, the number of children included in this study was small. Additionally, our study did not compare the systemic effects of IVB and LT.
Therefore, deferred LT following a single IVB promoted revascularization of immature retinas during the deferred window period. Moreover, combination therapy may decrease the number of injections required and follow-up visits.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: SJL. Data curation: KYN, JSL. Formal analysis: SJL. Methodology: Ji Eun Lee, Joo Eun Lee, HWK. Project administration: SJL. Supervision: SJL. Validation: SJL. Visualization: KYN, JSL Writing - original draft: SJL, KYN. Writing - review and editing: Ji Eun Lee, SJL. Approval of final manuscript: all authors.