Articles
- Page Path
- HOME > Kosin Med J > Volume 36(2); 2021 > Article
-
Case Reports
The Importance of Lamina Size Measurement and Proper Implants Selection before Laminoplasty : Two Case Reports - Dong Hwan Kim, Su Hun Lee, Dong Ha Kim, Kyoung Hyup Nam, In Ho Han, Byung Kwan Choi
-
Kosin Medical Journal 2021;36(2):169-174.
DOI: https://doi.org/10.7180/kmj.2021.36.2.169
Published online: December 31, 2021
1Department of Neurosurgery & Medical Research Institue, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Republic of Korea
2Department of Neurosurgery, Dong-Eui Hospital, Busan, Republic of Korea
3Department of Neurosurgery Pusan National University Yangsan Hospital, Yangsan, Republic of Korea
- Corresponding Author: Byung Kwan Choi, Department of Neurosurgery, Pusan National University Hospital, 179, Gudeok-Ro, Seo-Gu, Busan 49241, Republic of Korea, Tel: +82-51-240-7257, Fax: +82-51-244-0282, E-mail: spine@pusan.ac.kr
Copyright © 2021 by Korean Association of Medical Journal Editors
Articles published in Kosin Medical Journal are open-access, distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,187 Views
- 12 Download
Abstract
-
- Open door laminoplasty using plates is a safe and effective procedure for multi-level cord compression. To achieve stable laminar arch, various types of plate have been developed and used. Now, we introduce two rare complications related to the laminar shelf of plate.
- In the first case, we used the wider laminar shelf plate because the elevated lamina did not fit well into the usual laminar shelf. During follow-up, cord compression due to laminar shelf was observed.
- And in the second case, the laminar shelf of plate did not fit into the elevated lamina, so we inserted it with a little bit of force. But the patient’s symptom was not improved. On CT image, the inner cortical bone of the lamina was fractured.
- To prevent these complications, surgeons need to consider the thickness of the lamina and the size of the laminar shelf before surgery.
- CASE 1
- A 56 years old man with no medical history visited with gait disturbance that started one month ago. Neurological examination revealed upper arm radiating pain that did not follow definite dermatome and upper motor neuron signs such as abnormal tandem gait, a positive sign of Hoffman, Babinski, and Lhermitte.
- Ossification of the posterior longitudinal ligament (OPLL) from C4 to C7 with myelopathy was diagnosed on magnetic resonance imaging (MRI) and computer tomography (CT). So open-door laminoplasty using the plates was performed from C4 to C7. At surgery, we used a plate with wider laminar shelf, since the elevated spinal lamina did not enter the laminar shelf of the plate well.
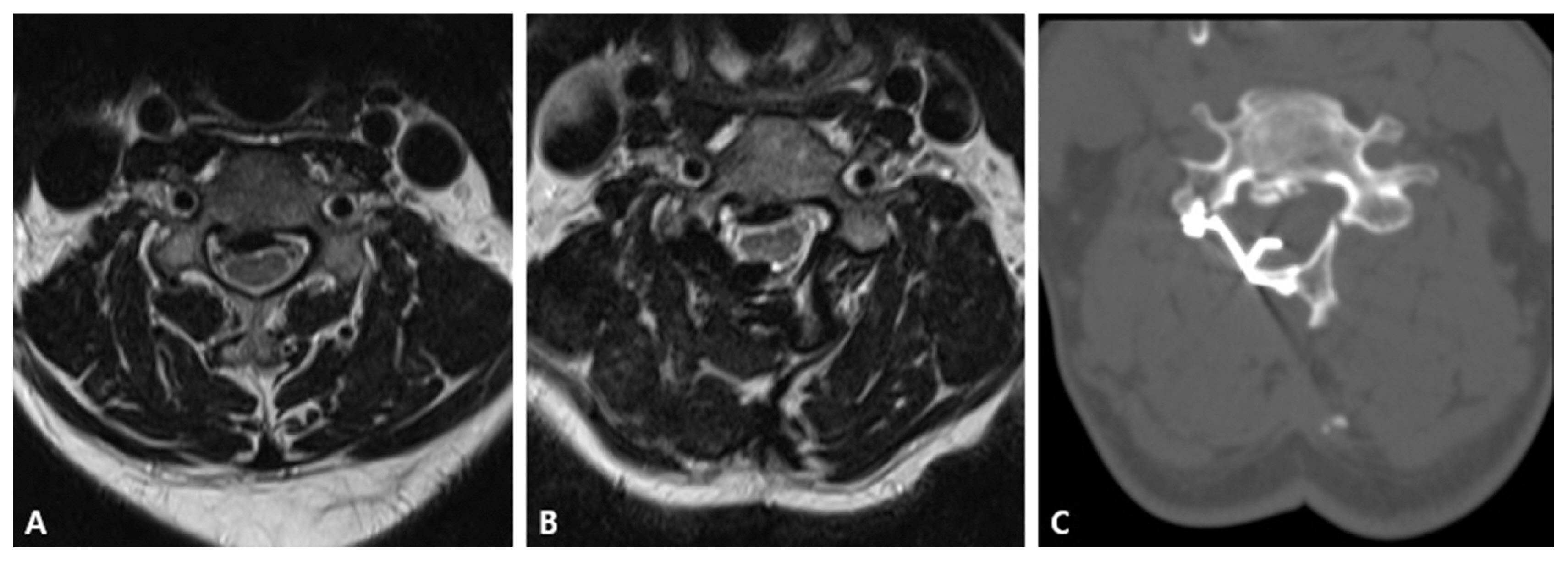
- During follow-up one year after surgery, the patient’s symptom had not improved so we conducted imaging evaluation. In MRI and CT, cord compression due to shelf of plate was observed (Fig. 1), so the plate was changed. Unfortunately, there was no obvious improvement in symptoms after revision surgery.
- CASE 2
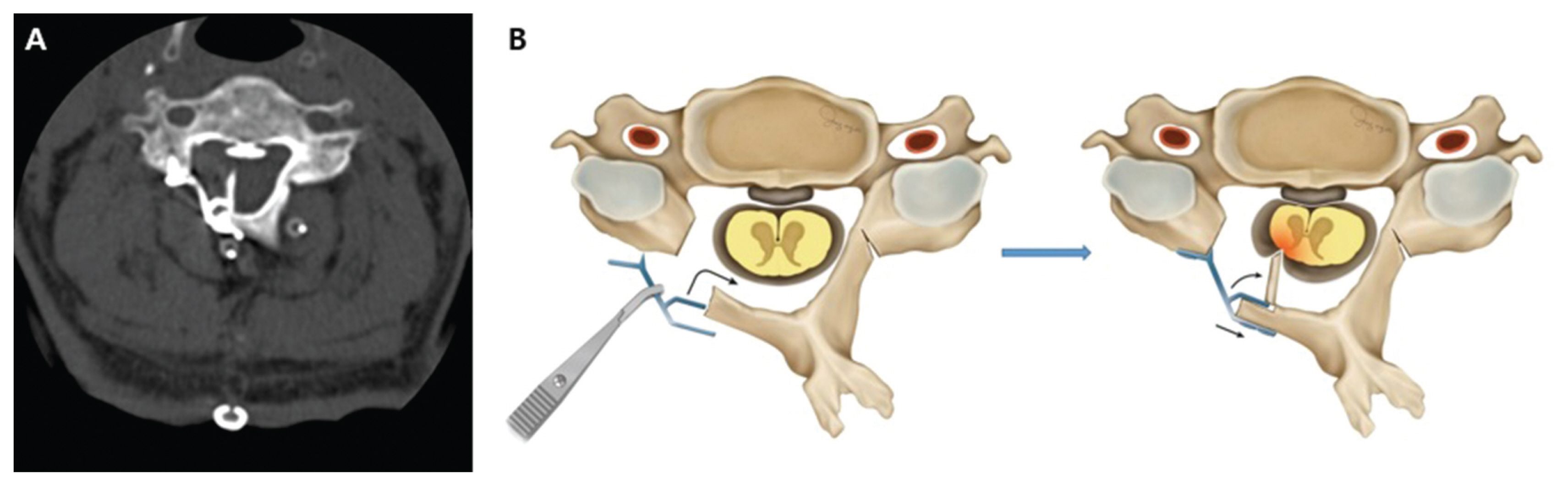
- A 71 years old man with lung cancer was referred for gait disturbance and right leg weakness. On physical examination, motor grade of the right leg was grade 3 and upper motor neuron signs were revealed. On MRI, segmental OPLL from C2 to C5 with myelopathy was diagnosed and laminoplasty was performed. The shelf of the plate did not fit into the elevated spinal lamina, so we inserted it with a little bit of force. After surgery, there was no improvement in the patient’s symptoms. So we conducted imaging evaluation. On CT, we identified that the inner cortical bone of the lamina was fractured, and spinal cord was compressed by the fractured fragment (Fig. 2). Reoperation for fractured inner cortical bone removal and plate reposition was performed. Two weeks after surgery, the patient’s right lower leg motor grade was restored to grade 4.
CASE
- Among various methods of laminoplasty, unilateral open-door laminoplasty, introduced by Hirabayashi et al., has been considered easy and safe procedure because of its indirect decompression of the spinal cord and it provides sufficient space for the spinal cord to drift away from a osteophyte, OPLL or herniated disc.9
- There are various methods for unilateral open-door laminoplasty. Suture system is always present with potential risk of closure of the open lamina due to lack of rigid fixation.3,10 There are also spacer systems such as bone struts, hydroxyapatite, and glass ceramic to prevent closure of lamina.4,6 However, spacers are not rigidly fixed, and risk of spacer dislocation exists. This dislocation may cause door reclosure as well as injury of the spinal cord or nerve root.11 In recent years, titanium plate fixation system has been developed in open-door laminoplasty. Compared to suture and spacer fixation, the plate system provides more rigid support and preservation of an enlarged spinal canal.9
- Among many plate fixation systems, plate with laminar shelf is the most commonly used. That plate has two special parts of design. First, a laminar shelf of plate allows for easy fixation to the cut edge of the lamina. And there is plate with wider laminar shelf to accommodate thick lamina comfortably. Second, kickstand design of plate allows it to be placed on the cut edge of the lateral mass stably (Fig. 3). So open door laminoplasty using the plate with laminar shelf has been a feasible method to resolve reclosure of the lamina and spacer dislocation issues.
- Common reports on complications of laminoplasty have been wound infections, post-operative neck pain, post-operative kyphosis, hinge fracture and C5 nerve palsy. However, instrumentation- related complications have been rare.12 Gabriel Liu et al.13 reported laminar screw back-out cases in laminoplasty, however, it did not associate with plate dislodgement or neurological complications. Chen et al.14 reported facet joint disturbance induced by mini-screws in plated cervical laminoplasty. This complication may not influence neurological recovery and spinal canal expansion. But in our cases, patients’ symptoms did not improve after surgery, and the patient with inner cortical bone fracture of lamina was observed to get worse.
- Unilateral open-door laminoplasty is relatively easy to perform, but careful attention should be practiced to avoid complications such as ours, especially in the less experienced surgeons. It is advisable to check the thickness of lamina before surgery and consider the laminar shelf size of the plate to be used in advance. When using a plate with wide laminar shelf, it is necessary to consider if spinal cord compression will be caused by the shelf of the plate. And when the cut edge of the lamina does not fit naturally into the shelf of the plate, it is also necessary to consider the possibility of inner cortex fracture of the lamina. Additionally, patient’s post-operative neurologic symptom get worse, it is important to evaluate the imaging test such as CT or MRI.
DISCUSSION
Acknowledgments
ACKNOWLEDGEMENTS
-
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Article information



- 1. Hur JW, Park YK, Kim BJ, Moon HJ, Kim JH. Risk Factors for Delayed Hinge Fracture after Plate-Augmented Cervical Open-Door Laminoplasty. J Korean Neurosurg Soc 2016;59:368–73.ArticlePubMedPMC
- 2. Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8:693–9.ArticlePubMed
- 3. Chen HC, Chang MC, Yu WK, Wang ST, Liu CL, Chen TH. Lateral mass anchoring screws for cervical laminoplasty: preliminary report of a novel technique. J Spinal Disord Tech 2008;21:387–92.PubMed
- 4. Goto T, Ohata K, Takami T, Nishikawa M, Tsuyuguchi N, Morino M, et al. Hydroxyapatite laminar spacers and titanium mini-plates in cervical laminoplasty. J Neurosurg 2002;97:323–9.ArticlePubMed
- 5. Lin X, Chen K, Tang H, Huang X, Wei C, Xiao Z. Comparison of anchor screw fixation versus mini-plate fixation in unilateral expansive open-door laminoplasty for the treatment of multi-level cervical spondylotic myelopathy. Medicine (Baltimore) 2018;97:e13534.Article
- 6. Nakano K, Harata S, Suetsuna F, Araki T, Itoh J. Spinous Process-Splitting Laminoplasty Using Hydroxyapatite Spinous Process Spacer. Spine 1992;17:S41–S3.ArticlePubMed
- 7. Lee DG, Lee SH, Park SJ, Kim ES, Chung SS, Lee CS, et al. Comparison of surgical outcomes after cervical laminoplasty: open-door technique versus French-door technique. J Spinal Disord Tech 2013;26:E198–203.PubMed
- 8. Park AE, Heller JG. Cervical laminoplasty: use of a novel titanium plate to maintain canal expansion--surgical technique. J Spinal Disord Tech 2004;17:265–71.PubMed
- 9. Wang LN, Wang L, Song YM, Yang X, Liu LM, Li T. Clinical and radiographic outcome of unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation for cervical compressive myelopathy: a five-year follow-up study. Int Orthop 2016;40:1267–74.ArticlePubMed
- 10. Wang HQ, Mak KC, Samartzis D, El-Fiky T, Wong YW, Luo ZJ, et al. “Spring-back” closure associated with open-door cervical laminoplasty. Spine J 2011;11:832–8.ArticlePubMed
- 11. Kanemura A, Doita M, Iguchi T, Kasahara K, Kurosaka M, Sumi M. Delayed dural laceration by hydroxyapatite spacer causing tetraparesis following double-door laminoplasty. J Neurosurg Spine 2008;8:121–8.ArticlePubMed
- 12. Derenda M, Kowalina I. Cervical laminoplasty--review of surgical techniques, indications, methods of efficacy evaluation, and complications. Neurol Neurochir Pol 2006;40:422–32. discussion 33.PubMed
- 13. Liu G, Buchowski JM, Riew KD. Screw Back-Out Following “Open-Door” Cervical Laminoplasty: A Review of 165 Plates. Asian Spine J 2015;9:849–54.ArticlePubMedPMC
- 14. Chen H, Li H, Wang B, Li T, Gong Q, Song Y, et al. Facet joint disturbance induced by miniscrews in plated cervical laminoplasty: Dose it influence the clinical and radiologic outcomes? Medicine (Baltimore) 2016;95:e 4666.
References
Figure & Data
References
Citations


 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite