Articles
- Page Path
- HOME > Kosin Med J > Volume 31(2); 2016 > Article
-
Original Article
Prognostic Significance of Neutrophil Lymphocyte Ratio and Platelet Lymphocyte Ratio in Diffuse Large B-Cell Lymphoma Patients Treated with R-CHOP - Lee Chun Park, Ho Sup Lee, Eun Mi Lee, Seong Hoon Shin, Yang Soo Kim
-
Kosin Medical Journal 2016;31(2):122-133.
DOI: https://doi.org/10.7180/kmj.2016.31.2.122
Published online: January 20, 2016
Department of Internal Medicine, College of Medicine, Kosin University, Busan, Korea
- Corresponding Author: Yang Soo Kim, Department of Internal Medicine, College of Medicine, Kosin University, 262, Gamcheon-ro, Seo-gu, Busan 49267, Korea Tel: +82-51-990-5820 Fax: +82-51-990-5820 E-mail: 2000p@hanmail.net
• Received: January 9, 2015 • Accepted: June 3, 2015
Copyright © 2016 Kosin University School of Medicine Proceedings
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,009 Views
- 1 Download
- 1 Crossref
Abstract
-
Objectives
- The both values of neutrophil lymphocyte ratio (NLR) and platelet lymphocyte ratio (PLR) were reported as indexes of systemic inflammation and readily available and inexpensive prognostic markers in patients with solid cancer. The objective of this study was to clarify whether the NLR and PLR were significant prognostic markers in Korean diffuse large B-cell lymphoma (DLBCL) patients treated with R-CHOP as a first line therapy.
-
Methods
- : We retrospectively collected the clinical data of ninety nine DLBCL patients treated with R-CHOP from 2004 to 2012 and analyzed. NLR and PLR were calculated from complete blood count (CBC) and differential leukocyte count.
-
Results
- : In univariate analysis, NLR was significantly associated with 5-year progression free survival(PFS) rate (P= 0.039), but not significantly associated with 5-year overal survival (OS) rate (P= 0.276). PLR was not significantly associated with 5-year PFS (P= 0.632) and OS rate (P= 0.855). In multivariate analysis, NLR was not a significant independent prognostic factor for 5-year PFS (P= 0.415) and OS rate (P= 0.991).
-
Conclusion
- : The NLR can be considered a useful predictor of survival outcome. The PLR is not a valid predictor of survival outcome.
Fig. 1.Five years progression free survival curves and overall survival curves according to Neutrphil/lymphocyte ratio in patients with diffuse large B-cell lymphoma. a. Five years progression free survival curves b. Five years overall survival curves
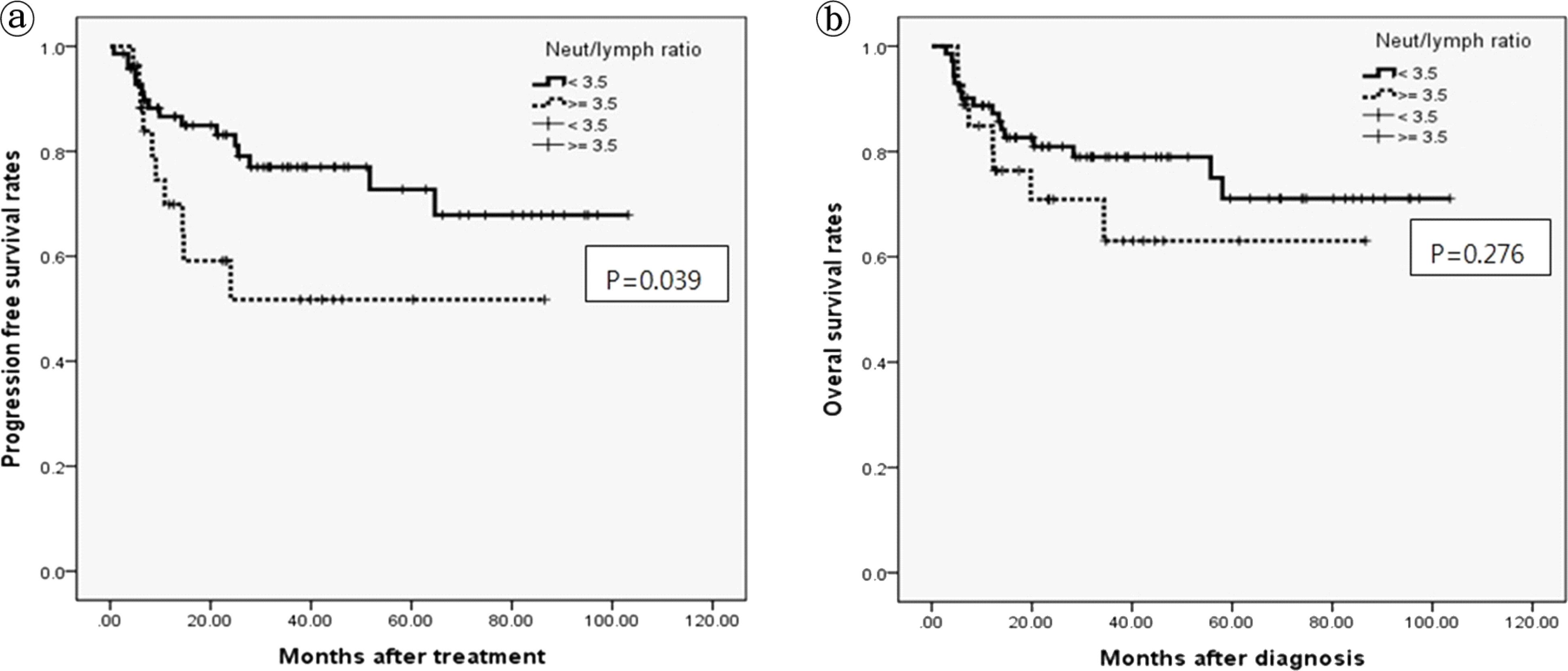
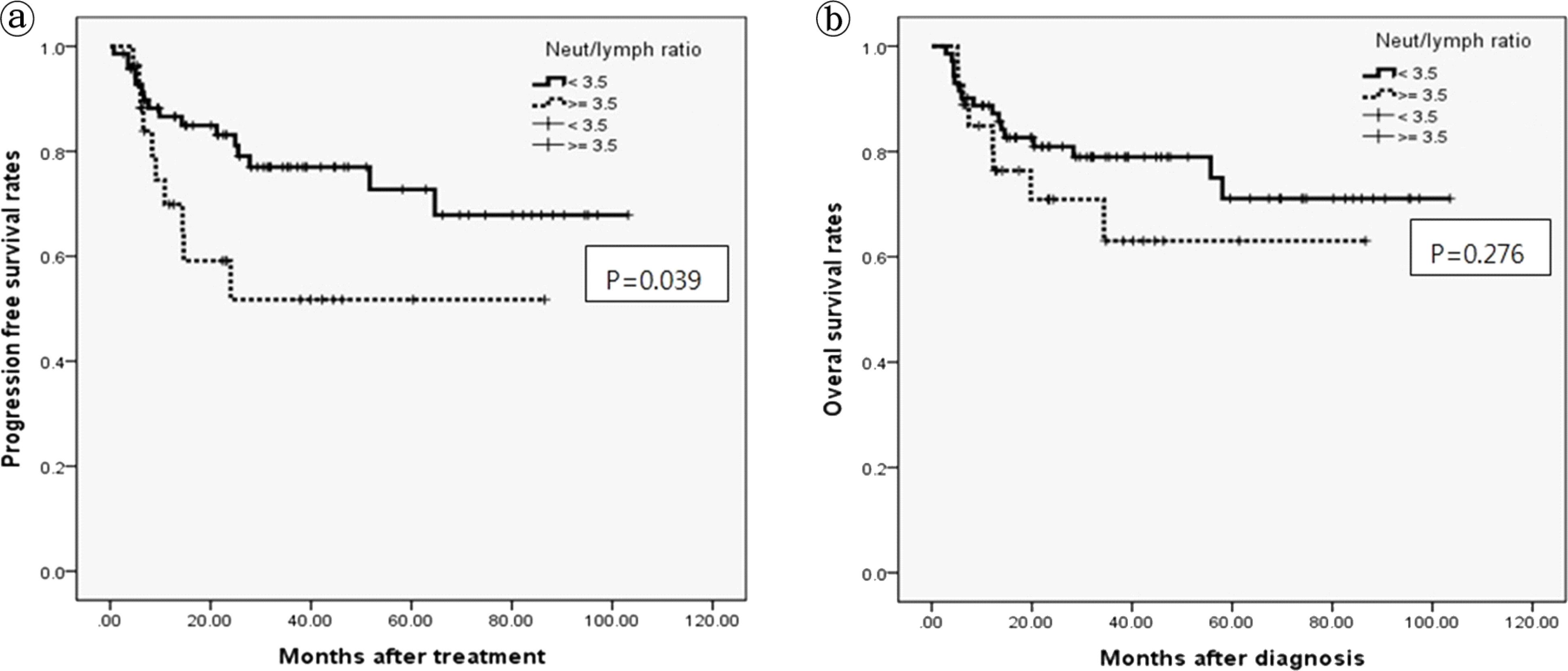
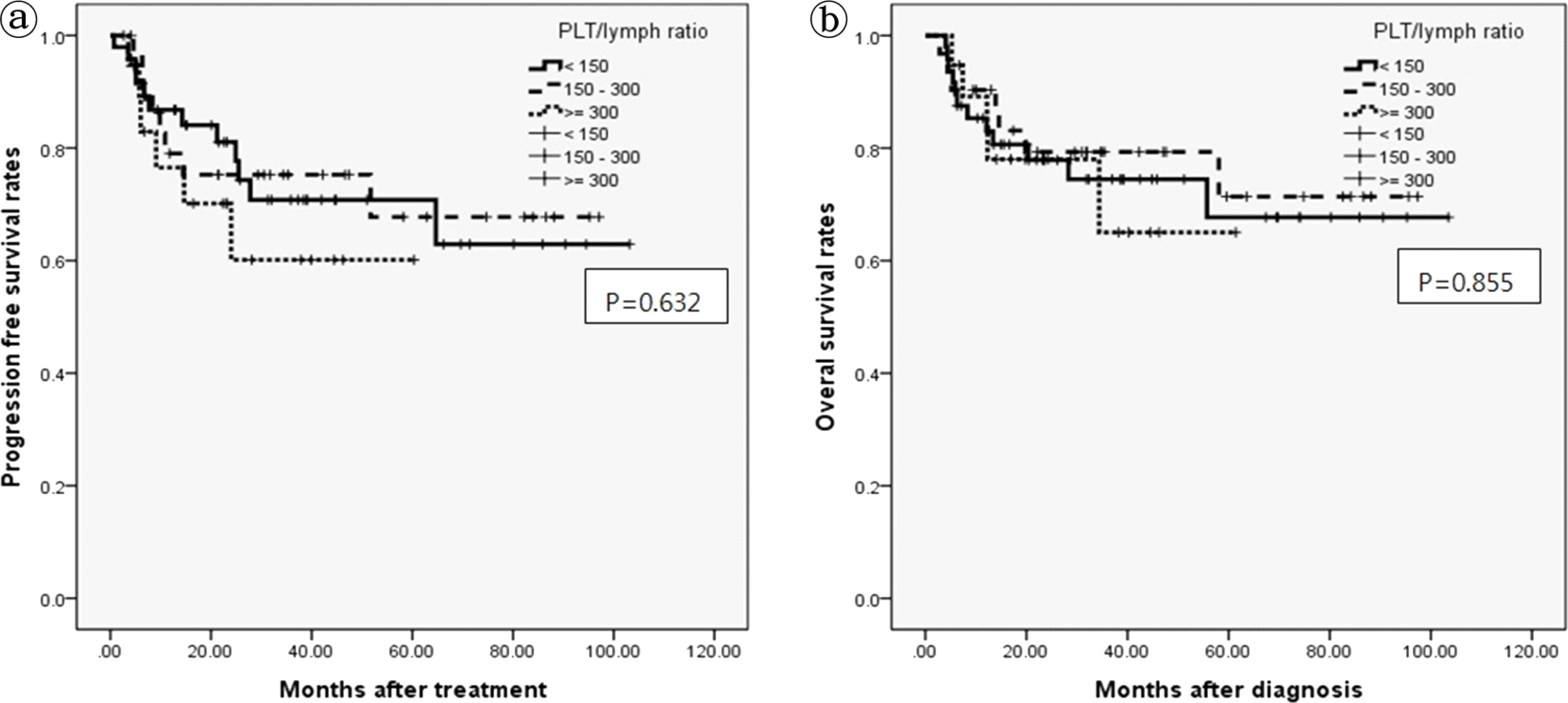
Fig. 2.Five years progression free survival curves and overall survival curves according to Platelet/lymphocyte ratio in patients with diffuse large B-cell lymphoma. a. Five years progression free survival curves b. Five years overall survival curves
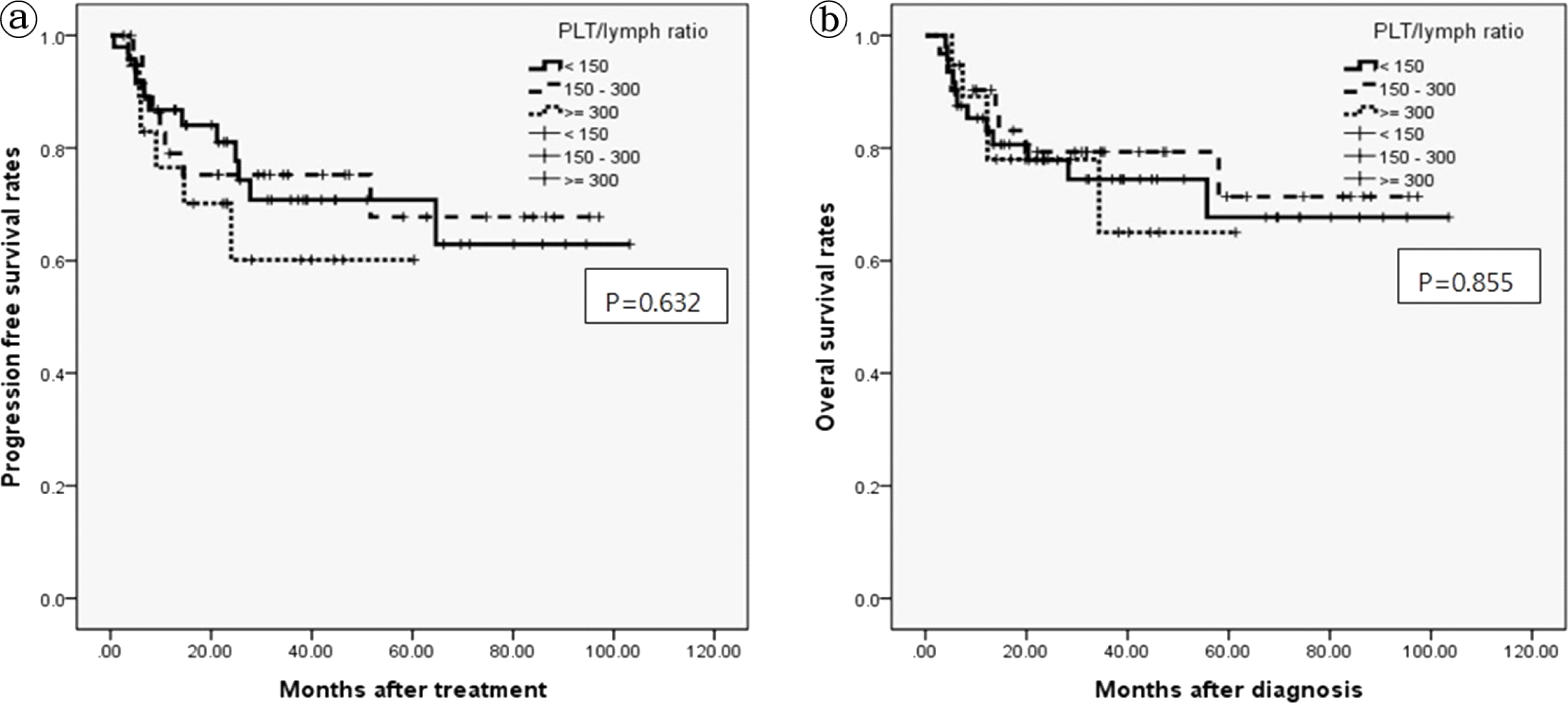
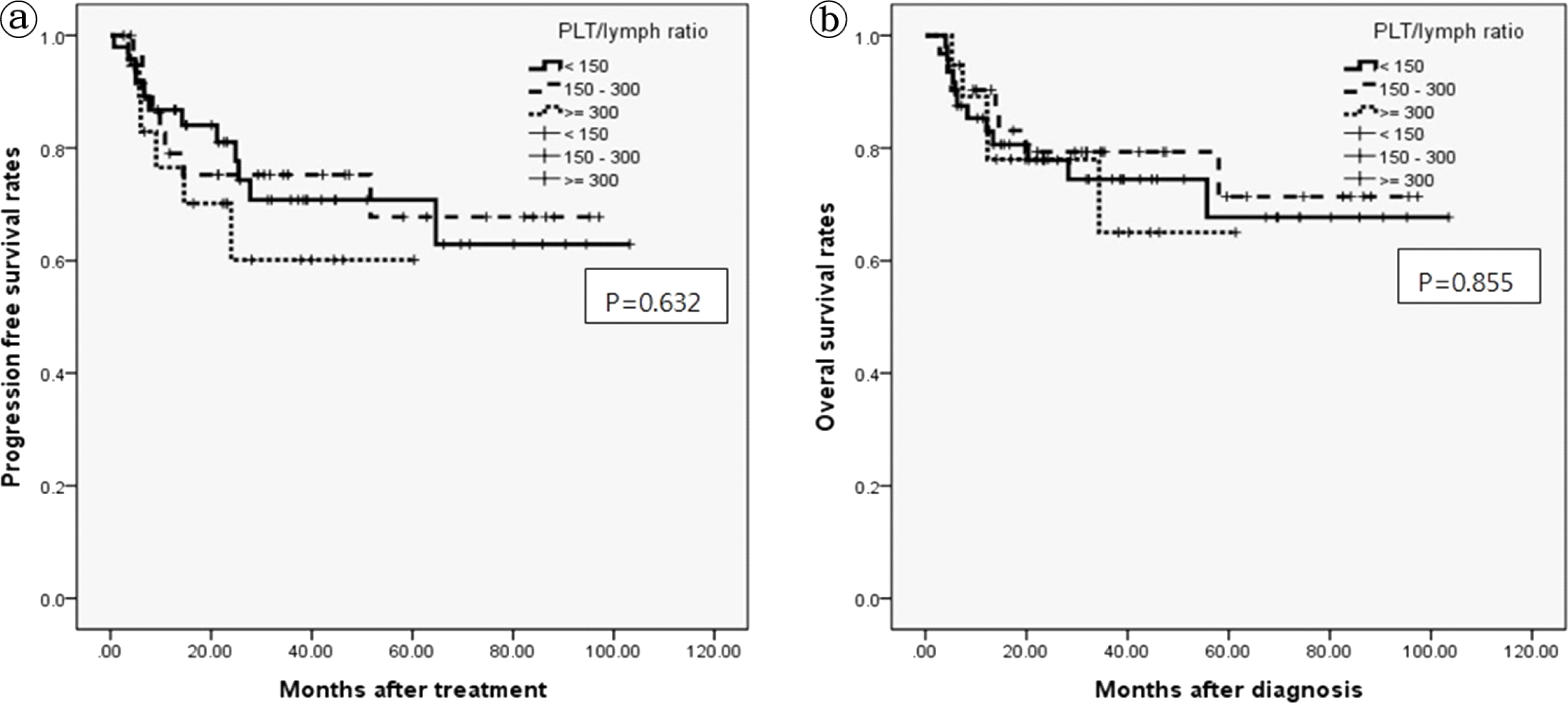
Table 1.Patient characteristics
Table 2.Prognostic factors for survival in patients with DLBCL by univariate analysis
Table 3.Independent prognostic factors for survival in patients with DLBCL by multivariate analysis
- 1. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature 2008;454:436–44.ArticlePubMed
- 2. Coussens LM, Werb Z. Inflammation and cancer. Nature 2002;420:860–7.ArticlePubMedPMC
- 3. DeNardo DG, Andreu P, Coussens LM. Interactions between lymphocytes and myeloid cells regulate pro-versus antitumor immunity. Cancer Metastasis Rev 2010;29:309–16.ArticlePubMedPMC
- 4. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell 2010;140:883–99..Article
- 5. Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol 2010;6:149–63.ArticlePubMed
- 6. Kim DK, Oh SY, Kwon HC, Lee S, Kwon KA, Kim BG, et al. Clinical significances of preoperative serum interleukin-6 and C-reactive protein level in operable gastric cancer. BMC Cancer 2009;9:155.ArticlePubMedPMC
- 7. Crumley AB, McMillan DC, McKernan M, McDonald AC, Stuart RC. Evaluation of an inflammation-based prognostic score in patients with inoperable gastro-oesophageal cancer. Br J Cancer 2006;94:637–41.ArticlePubMedPMC
- 8. Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer 2011;104:1288–95.ArticlePubMedPMC
- 9. Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F, et al. Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg 2009;197:466–72.ArticlePubMed
- 10. Engelken FJ, Bettschart V, Rahman MQ, Parks RW, Garden OJ. Prognostic factors in the palliation of pancreatic cancer. Eur J Surg Oncol 2003;29:368–73.ArticlePubMed
- 11. McMillan DC, Elahi MM, Sattar N, Angerson WJ, Johnstone J, McArdle CS. Measurement of the systemic inflammatory response predicts cancer-specific and non-cancer survival in patients with cancer. Nutr Cancer 2001;41:64–9.ArticlePubMed
- 12. Bachelot T, Ray-Coquard I, Catimel G, Ardiet C, Guastalla JP, Dumortier A, et al. Multivariable analysis of prognostic factors for toxicity and survival for patients enrolled in phase I clinical trials. Ann Oncol 2000;11:151–6.ArticlePubMed
- 13. Viganó A, Bruera E, Jhangri GS, Newman SC, Fields AL, Suarez-Almazor ME. Clinical survival predictors in patients with advanced cancer. Arch Intern Med 2000;160:861–8.ArticlePubMed
- 14. O'Mahony JB, Palder SB, Wood JJ, Mclrvine A, Rodrick ML, Demling RH, et al. Depression of cellular immunity after multiple trauma in the absence of sepsis. J Trauma 1984;24:869–75.ArticlePubMed
- 15. O'Gorman P, McMillan DC, McArdle CS. Prognostic factors in advanced gastrointestinal cancer patients with weight loss. Nutr Cancer 2000;37:36–40.ArticlePubMed
- 16. Sierko E, Wojtukiewicz MZ. Platelets and angiogenesis in malignancy. Semin Thromb Hemost 2004;30:95–108.ArticlePubMed
- 17. Alexandrakis MG, Passam FH, Moschandrea IA, Christophoridou AV, Pappa CA, Coulocheri SA, et al. Levels of serum cytokines and acute phase proteins in patients with essential and cancer-related thrombocytosis. Am J Clin Oncol 2003;26:135–40.ArticlePubMed
- 18. Klinger MH, Jelkmann W. Role of blood platelets in infection and inflammation. J Interferon Cytokine Res 2002;22:913–22.PubMed
- 19. He W, Yin C, Guo G, Jiang C, Wang F, Qiu H, et al. Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. Med Oncol 2013;30.Article
- 20. Bhatti I, Peacock O, Lloyd G, Larvin M, Hall RI. Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus platelet-lymphocyte ratio. Am J Surg 2010;200:197–203.ArticlePubMed
- 21. Kwon HC, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ, et al. Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 2012;17:216–22.ArticlePubMed
- 22. Cox MC, Nofroni I, Laverde G, Ferrari A, Amodeo R, Tatarelli C, et al. Absolute lymphocyte count is a prognostic factor for diffuse large B-cell lymphoma. Br J Haematol 2008;141:265–8.ArticlePubMed
- 23. Oki Y, Yamamoto K, Kato H, Kuwatsuka Y, Taji H, Kagami Y, et al. Low absolute lymphocyte count is a poor prognostic marker in patients with diffuse large B-cell lymphoma and suggests patients survival benefit from rituximab. Eur J Haematol 2008;81:448–53.ArticlePubMed
- 24. Kim DH, Baek JH, Chae YS, Kim YK, Kim HJ, Park YH, et al. Absolute lymphocyte counts predicts response to chemotherapy and survival in diffuse large B-cell lymphoma. Leukemia 2007;21:2227–30.ArticlePubMed
- 25. Porrata LF, Ristow K, Habermann T, Inwards DJ, Micallef IN, Markovic SN. Predicting survival for diffuse large B-cell lymphoma patients using baseline neutrophil/lymphocyte ratio. Am J Hematol 2010;85:896–9.ArticlePubMed
- 26. MacDonald N. Cancer cachexia and targeting chronic inflammation: a unified approach to cancer treatment and palliative/supportive care. J Support Oncol 2007;5:157–62.PubMed
- 27. Maltoni M, Caraceni A, Brunelli C, Broeckaert B, Christakis N, Eychmueller S, et al. Prognostic factors in advanced cancer patients: evience -based clinical recommendations–a study by the Steering Committee of the European Association for Palliative Care. J Clin Oncol 2005;23:6240–8.PubMed
- 28. Salazar-Onfray F, López MN, Mendoza-Naranjo A. Paradoxical effects of cytokines in tumor immune surveillance and tumor immune escape. Cytokine Growth Factor Rev 2007;18:171–82.ArticlePubMed
References
Figure & Data
References
Citations
Citations to this article as recorded by 

- Prognostic role of neutrophil-to-lymphocyte ratio in diffuse large B cell lymphoma patients: an updated dose–response meta-analysis
Shidai Mu, Lisha Ai, Fengjuan Fan, You Qin, Chunyan Sun, Yu Hu
Cancer Cell International.2018;[Epub] CrossRef

 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite