Articles
- Page Path
- HOME > Kosin Med J > Volume 37(3); 2022 > Article
-
Case report
Secondary hyperparathyroidism due to multiple parathyroid carcinomas in a patient with chronic hemodialysis: a case report -
Soree Ryang1
 , Wook Yi1
, Wook Yi1 , Mijin Kim1
, Mijin Kim1 , Sang Heon Song2
, Sang Heon Song2 , Byung Joo Lee3
, Byung Joo Lee3 , Bo Hyun Kim1
, Bo Hyun Kim1
-
Kosin Medical Journal 2022;37(3):255-259.
DOI: https://doi.org/10.7180/kmj.22.103
Published online: July 27, 2022
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Pusan National University Hospital, Busan, Korea
2Division of Nephrology, Department of Internal Medicine, Pusan National University Hospital, Busan, Korea
3Department of Otorhinolaryngology-Head and Neck Surgery, Pusan National University Hospital, Busan, Korea
- Corresponding Author: Bo Hyun Kim, MD, PhD Division of Endocrinology and Metabolism, Department of Internal Medicine, Biomedical Research Institute, Pusan National University Hospital, 179 Gudeok-ro, Seo-gu, Busan 49241, Korea Tel: +82-51-240-7236 Fax: +82-51-254-3237 E-mail: pons71@hanmail.net
Copyright © 2022 Kosin University College of Medicine.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,325 Views
- 22 Download
Abstract
- Parathyroid carcinoma (PC) in cases of secondary or tertiary hyperparathyroidism is relatively uncommon, and only a few case reports have described this entity. Although some papers have reported patients with one or two parathyroid malignancies, multiple PC–especially three or more–have been even more rarely reported. Herein, we report a case of secondary hyperparathyroidism due to multiple PCs in a chronic hemodialysis patient. A 54-year-old man with end-stage kidney disease was referred for hyperparathyroidism. He had been diagnosed with chronic kidney disease in 2001 and had begun hemodialysis in 2009. In laboratory tests, intact parathyroid hormone (iPTH) was markedly elevated to 1,144.1 pg/mL (normal range: 15.0–68.3 pg/mL) and serum calcium was mildly elevated to 10.56 mg/dL (normal range: 8.5–10.3 mg/dL). Ultrasonography showed hypoechoic nodules in the posterior part of both thyroid glands. All three nodules showed increased uptake on a 99mTc sestamibi scan. The patient underwent total parathyroidectomy with autotransplantation to the right forearm. Histopathology findings showed three PCs with capsular invasion and one parathyroid hyperplasia. In the immediate postoperative period, the iPTH level dropped from 1,446.8 to 82.4 pg/dL and, after 1 month, to 4.0 pg/dL. This patient needed oral calcium carbonate and active vitamin D to maintain appropriate serum calcium levels. Although multiple PCs are rare, they can cause secondary hyperparathyroidism. Therefore, clinicians should suspect multiple PCs when patients’ serum iPTH levels are exceptionally high. Additionally, since PCs could occur in multiple glands, autotransplantation of the parathyroid gland after parathyroidectomy should be done carefully.
- Parathyroid carcinoma (PC) is one of the rarest endocrine malignancies [1]. It is known to cause 0.5% to 5% of primary hyperparathyroidism (HPT) and usually develops in patients aged between 40 and 50 with no gender preference [2,3].
- Secondary HPT is one of the common complications in patients with chronic kidney disease (CKD). In CKD patients, decreased activation of vitamin D causes hypocalcemia and hyperphosphatemia, which leads to overproduction of parathyroid hormone [4]. Most of the PC cases are associated with primary HPT, however, there are few cases of PC are combined with secondary or tertiary HPT. In this paper, we report a rare case of secondary HPT due to multiple PC in a patient with CKD.
Introduction
- Ethical statements: This study was approved by the Ethics Committee of Pusan National University Hospital (No. 2204-008-113). Written informed consent from patient was obtained.
- 1. Medical history
- A 54-year-old man with end-stage renal disease was referred to the endocrinology department due to markedly elevated serum intact parathyroid hormone (iPTH) level. He had been diagnosed with CKD in 2001 and started hemodialysis in 2009. He showed no symptoms related to HPT. A bone mineral density showed a T score of 0.6 in the spine, −1.7 in the femur neck and −0.9 for total hip, consistent with osteopenia (distal forearm was not evaluated at initial). As he had no history of parathyroid or bone disease, and was subsequently diagnosed with secondary HPT. The patient was taking several medications including sevelamer carbonate (phosphate binder), cinacalcet (calcimimetics) or paricalcitol (vitamin D receptor activator) injections. Though his serum calcium level was mildly elevated and there was no evidence of renal stone or severe bone disease, we recommended him to have parathyroid surgery because of large size of parathyroid glands and elevated iPTH which was not controlled by the medication. He was and underwent a total parathyroidectomy.
- 2. Laboratory and imaging studies
- As a potential kidney transplantation recipient, blood tests and routine imaging studies were performed in the Nephrology department. Initial iPTH was markedly elevated to 1,144.1 pg/mL (reference range: 15.0–68.3 pg/mL) while there was a mild elevation of serum calcium level to 10.56 mg/dL (reference range: 8.5–10.3 mg/mL).
- Other laboratory data (with reference ranges) were as follows: albumin 4.60 (3.3–5.2) mg/dL, phosphorous 3.66 (2.0–4.6) mg/dL, creatinine 11.59 (0.4–1.2) mg/dL, hemoglobin 11.4 (13.5–17.5) g/dL, thyroid stimulating hormone 0.69 (0.3–0.5) μIU/mL, 25-OH vitamin D3 19.16 (30–150 ng/mL). Ultrasonography of the thyroid and parathyroid showed 0.62×0.77 cm hypoechoic nodule with well-defined margin at posterior of right thyroid gland, 1.20×1.94 cm and 1.91×1.79 cm hypoechoic nodules with irregular margin and inhomogeneous internal echo at posterior of left thyroid gland which were suspected to be parathyroid lesions (Fig. 1A-C). On 99mTc-sestamibi parathyroid single photon emission computed tomography, all of the three nodules persistently showed increased uptake after 2 hours of intravenous 99mTc sestamibi injection (Fig. 1D).
- 3. Surgery and postsurgical histopathology
- The patient underwent total parathyroidectomy with autotransplantation on his right forearm. Right superior, right inferior, left superior, left inferior parathyroid glands were all removed. Since intraoperative gross observation of right inferior parathyroid gland was fairly smaller than that of other masses, and frozen biopsy showed no malignancy, this tissue was auto-transplanted on the patient's right forearm.
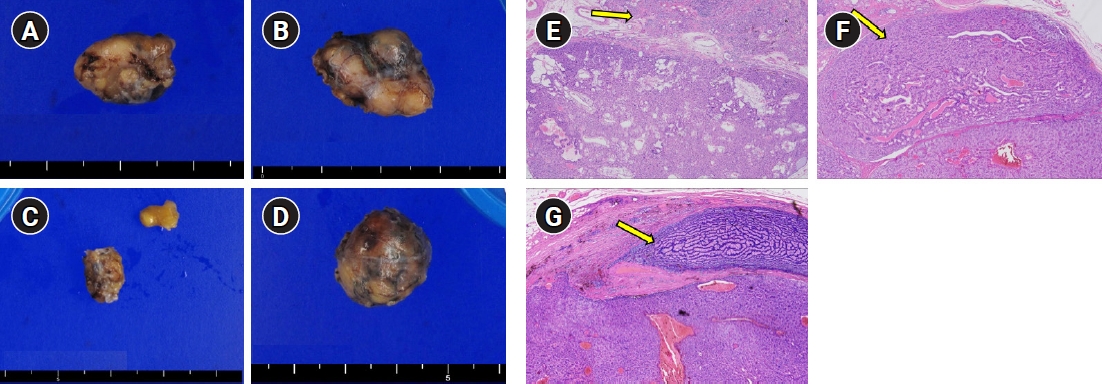
- The final histopathology report revealed three PC with capsular invasion (1.5×1.2×1.0 cm at right superior, 2.2×1.7×1.0 cm at left superior, and 2.2×1.7×1.5 cm at left inferior parathyroid glands). The right inferior parathyroid mass showed parathyroid hyperplasia (Fig. 2).
- 4. Postoperative course
- Postoperative laboratory results showed noticeably dropped iPTH from 1,446.8 to 82.4 pg/dL and gently dropped serum calcium level from 10.49 to 9.20 mg/dL. Serum phosphorous level after parathyroidectomy was changed from 2.18 mg/dL to 4.88 mg/dL. During the postoperative period, the patient's biochemical results exhibited postsurgical hypocalcemia (iPTH 4.0 pg/dL and serum calcium 6.46 mg/dL) and the patient was discharged with calcium carbonate and oral active vitamin D supplements.
Case
- In this paper, we presented a case of multiple PCs with secondary HPT. Secondary HPT is one of the most frequent complications in patients with chronic hemodialysis. However, we rarely encounter secondary HPT which is caused by PC, since majority of the cases are due to parathyroid adenoma or hyperplasia. Considering that clinical presentation of PC is similar to that of benign primary HPT, preoperative diagnosis of PC from other benign parathyroid diseases is rather challenging [5]. Even parathyroid gland ultrasonography and 99mTc sestamibi scan do not provide definitive differential diagnosis between benign and malignant masses of parathyroid gland [6]. Low incidence of PC also makes it difficult to distinguish it from parathyroid adenoma or hyperplasia. In addition, for subjects who are on chronic hemodialysis, it is even more difficult to suspect PC before surgery than in patients with normal kidney disease. One of the reasons could be relatively low calcium level, due to hemodialysis and oral calcimimetics. Furthermore, continuous stimulating of four parathyroid glands owing to low serum vitamin D level can lead to high serum iPTH level, which can make the differential diagnosis of PC and benign diseases more complicated [7]. For these reasons, most PC cases are likely to be confirmed by histological examination after surgical removal of the tissue in patients with end-stage renal disease. Like benign parathyroid disease, signs and symptoms of PC can include hypercalcemia, bone and joint pain, osteoporosis, nephrolithiasis, renal and cardiac dysfunction [2]. However, PC tends to present with more severe course than benign parathyroid lesions. Referring to several literatures, severe hypercalcemia (>14 mg/dL), markedly elevated iPTH level, palpable neck mass (>3 cm) and significant renal or skeletal involvement may indicate features of PC [8,9]. In this case, initial serum calcium level was 10.56 mg/dL which was gently elevated. Possible causes could be hemodialysis, or oral cinacalcet which the patient had been taking.
- Generally, postsurgical hypocalcemia occurs more in patients with secondary HPT than in primary HPT [10], postoperative hypocalcemia or hungry bone syndrome should be carefully examined. This patient is also taking calcium and vitamin D supplements, on close observation. He had autotransplantation parathyroid gland on his right arm, and generally it takes 2 to 3 months for transplanted parathyroid become viable, he might need to maintain taking oral supplements for some periods.
- Multiple PC is a rare disease. Referring to the data from previous literature, multiple PC occurs infrequently, and there are just a few case reports [11,12]. In this case, the patient had three individual cancers developed from each parathyroid gland. Although we did not know those parathyroid lesions were malignant before the surgery, we readily decided to remove most of the sites of parathyroid glands because of the high iPTH level despite of maximal medical therapy. To some degree, it was an unexpected result that all of the three parathyroid lesions were cancerous. It is difficult to distinguish PC from benign diseases before surgery. Even fine-needle aspiration of the parathyroid mass is not recommended as it may cause tumor rupture and seeding [13]. Therefore, intraoperative findings are important to make the appropriate decision. The size, color (grayish-white), hardness, and soft tissue adherence could be the findings in high suspicion of carcinoma [5].
- Surgical resection is the mainstay of the treatment for PC, and en bloc resection is generally recommended, to bring the optimal prognosis [14]. Complete exploration of all four parathyroid glands and watchful inspection for adjacent structures can minimize the recurrence rate. According to previous study, patients who had been diagnosed PC preoperatively and underwent en bloc resection had a recurrence rate of 33%, while those who were diagnosed PC postoperatively and underwent suboptimal resection had a recurrence rate of 50% [15]. However, recognition of malignancy before or even during the surgery is not simple; only 12% of PC patients are reported to have en bloc resection [16]. Our patient also had not been diagnosed malignancy preoperatively, and extensive manipulation was not routinely done during the surgery. Further surveillance might be crucial in this patient.
- In this case, we presented an extraordinary case of secondary HPT with multiple PC in patient with chronic hemodialysis. Although it is rare, multiple PC can cause secondary HPT. Therefore, clinicians should suspect multiple PC when patient’s serum iPTH level is exceptionally high. Additionally, since PC could occur in multiple glands, autotransplantation of parathyroid gland after parathyroidectomy should be done carefully.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
This research was supported by a clinical research grant from Pusan National University Hospital in 2022.
-
Author contributions
Conceptualization: SR, WY, MK, BHK. Data curation: BJL, SHS. Methodology: MK. Project administration: BHK. Visualization: BJL. Writing-original draft: SR, WY. Writing-review & editing: SR, WY, MK, BHK. Approval of final manuscript: all authors.
Article information

- 1. McClenaghan F, Qureshi YA. Parathyroid cancer. Gland Surg 2015;4:329–38.ArticlePubMedPMC
- 2. Shane E. Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab 2001;86:485–93.ArticlePubMed
- 3. Belafsky PC. Current opinion in otolaryngology & head & neck surgery: editorial comment. Curr Opin Otolaryngol Head Neck Surg 2009;17:419.ArticlePubMed
- 4. Habas E Sr, Eledrisi M, Khan F, Elzouki AY. Secondary hyperparathyroidism in chronic kidney disease: pathophysiology and management. Cureus 2021;13:e16388.ArticlePubMedPMC
- 5. Machado NN, Wilhelm SM. Parathyroid cancer: a review. Cancers (Basel) 2019;11:1676.ArticlePubMedPMC
- 6. Cao J, Chen C, Wang QL, Xu JJ, Ge MH. Parathyroid carcinoma: a report of six cases with a brief review of the literature. Oncol Lett 2015;10:3363–8.ArticlePubMedPMC
- 7. Kada S, Tanaka M, Yasoda A. Parathyroid carcinoma in a patient with secondary hyperparathyroidism and thyroid hemiagenesis: a case report and review of the literature. Ear Nose Throat J 2021;Jul 28 https://doi.org/10.1177/01455613211036240.Article
- 8. Duan K, Mete O. Parathyroid carcinoma: diagnosis and clinical implications. Turk Patoloji Derg 2015;31 Suppl 1:80–97.ArticlePubMed
- 9. Kowalski GJ, Bednarczyk A, Bula G, Gawrychowska A, Gawrychowski J. Parathyroid carcinoma: a study of 29 cases. Endokrynol Pol 2022;73:56–63.ArticlePubMed
- 10. Wen P, Xu L, Zhao S, Gan W, Hou D, Zhang L, et al. Risk factors for severe hypocalcemia in patients with secondary hyperparathyroidism after total parathyroidectomy. Int J Endocrinol 2021;2021:6613659.ArticlePubMedPMCPDF
- 11. Haciyanli M, Oruk G, Ucarsoy AA, Gur O, Genc H, Krikorian A, et al. Multiglandular parathyroid carcinoma: case report and review of the literature. Endocr Pract 2011;17:598–601.ArticlePubMed
- 12. Oh SK, Park YH, Kim JH, Lee MS, Min HK. Multiple primary parathyroid carcinoma. J Korean Surg Soc 1990;39:546–53.
- 13. Harari A, Waring A, Fernandez-Ranvier G, Hwang J, Suh I, Mitmaker E, et al. Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab 2011;96:3679–86.ArticlePubMed
- 14. Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol 2012;13:11–23.ArticlePubMedPDF
- 15. Kebebew E. Parathyroid carcinoma. Curr Treat Options Oncol 2001;2:347–54.ArticlePubMedPDF
- 16. Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer 2007;109:1736–41.ArticlePubMed
References
Figure & Data
References
Citations


 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite


